2Department of Endocrinology, Memorial Hospital, Istanbul, Turkey
3Department of Thoracic Surgery, Yedikule Pulmonology and Thoracic Surgery Hospital, Istanbul, Turkey DOI : 10.26663/cts.2024.026
Summary
Background: We aimed to study the effects of subclinical hypothyroidism on patient satisfaction after hyperhidrosis surgery.Materials and Methods: Patients who underwent primary hyperhidrosis surgery from February 2013 to January 2017 were retrospectively evaluated and divided into two groups: Group 1 with normal thyroid function and Group 2 with subclinical hypothyroidism. All patients completed a postoperative satisfaction questionnaire on a 5-point Likert scale, with Cronbach’s Alpha reliability coefficients of 0.93 preoperatively and 0.96 postoperatively. The questionnaire assessed satisfaction differences between groups in daily life following surgery.
Results: A total of 82 patients aged 18-65 and met Hornberger’s criteria were evaluated in the study. Patient satisfaction rate was 80.5% for the overall population. Although the difference between preoperative and postoperative state was statistically significant (Greenhouse-Geisser; p < 0.0001), no statistically significant difference was found in postoperative satisfaction between Group 1 and Group 2. (p = 0.13).
Conclusions: Subclinical hypothyroidism does not impact the outcomes of endoscopic thoracic sympathectomy; thus, patients with this condition can safely undergo the procedure based on this study's findings.
Introduction
Sweating is a part of the thermoregulatory system. Hyperhidrosis is defined as excessive sweating and eccrine sweat glands working more than normal [1,2]. The most common form is primary hyperhidrosis and its clinical presentation is mostly localized as palmoplantar, axillary and facial in order of frequency [3]. Its exact incidence is not known, but it is thought to affect 0.6 to 2.8% of the population [4].Topical and systemic medical therapies can be used in the treatment as well as options such as iontophoresis and Botox, but surgical treatment is the gold standard [5,6].
Thyroid disorders, a common cause of secondary hyperhidrosis, should also be considered in cases of subclinical variants. Overt thyroid disorders can clearly cause secondary hyperhidrosis, and asymptomatic subclinical thyroid diseases may lead to unexpected skin conditions related to a flawed thermoregulatory system, potentially resulting in undesirable surgical outcomes [7]. In this study, we examined the relationship between subclinical hypothyroidism and its potential impact on hyperhidrosis surgery.
Subclinical hypothyroidism is a condition characterized by mildly elevated thyroid-stimulating hormone (TSH) levels while serum triiodothyronine (T3) and thyroxine (T4) levels remain within the normal range, and it is asymptomatic. The European Thyroid Association (ETA) guidelines for managing subclinical hypothyroidism were published nearly a decade ago, yet they remain valid, as the rationale for intervention - based on the patient's age, serum TSH levels, symptoms, and comorbidities - continues to be relevant today [8,9].
The impact of subclinical hypothyroidism on postoperative outcomes has been studied across various surgical specialties, but there is insufficient data regarding its effects on hyperhidrosis surgery. Although the association of hyperhidrosis and hyperthyroidism has been widely investigated, the relationship between hyperhidrosis surgery results and TSH levels has not been investigated before.
Methods
Patient Characteristics and Data CollectionThe study aimed to evaluate the link between hyperhidrosis and subclinical hypothyroidism regarding the patients’ overall postoperative satisfaction. This multisurgeon single-center retrospective study included all patients who underwent endoscopic thoracic sympathectomy between February 2013 and January 2017 in our hospital. The data of 82 patients who met Hornberger’s criteria [10] were analyzed in this study. The exclusion criteria were: 1) being out of the 18-65 age span, 2) abnormal preoperative TSH values, and 3) indications other than hyperhidrosis for surgery.
Patients were divided into two groups according to The American Association of Clinical Endocrinologists and The American Thyroid Association (ATA/AACE) Guidelines for Hypothyroidism in Adults which involves the TSH upper limit of The National Academy of Clinical Biochemistry (NACB) [8] as shown in Table 1. Group 1 was the patients with normal thyroid functions and Group 2 was the patients with subclinical hypothyroidism.
Table 1. TSH upper normal levels according to different study or society groups.
Preoperative TSH values of the patients were evaluated within the framework of the reference range of the biochemistry department of our hospital. Demographic information and hospital records such as operation reports were completely available for in-hospital study variables. Patients were contacted by phone or face-toface between January 3, 2018 and January 9, 2018, and a web-based (Google® Forms) questionnaire was administered (Figure 1), and the survey results were recorded. The questionnaire utilized in this study was adapted from the publication titled 'Questionnaire of Quality of Life in Patients with Primary Hyperhidrosis' [11]. It employs a 5-point Likert scale, with the instrument's reliability confirmed by Cronbach's Alpha coefficients of 0.93 before surgery and 0.96 after surgery, indicating a high level of reliability. The Institutional Ethical Committee approved the study protocol (HNEAH-KAEK 2017/551). The study conformed to the principles of the Declaration of Helsinki.
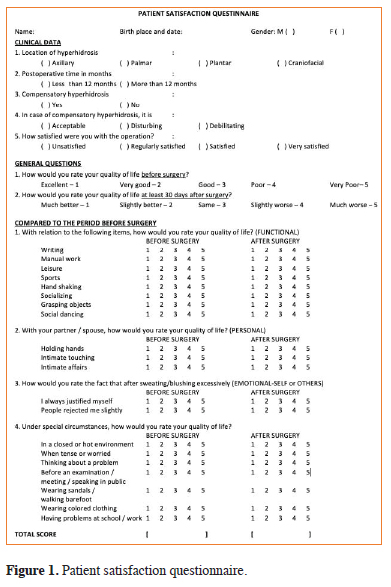 Click Here to Zoom |
Figure 1: Patient satisfaction questionnaire. |
Surgical Technique
All operations were performed with video-assisted
thoracoscopic surgery (VATS) technique. The patients
underwent double lumen intubation after appropriate
premedication. First the right and then left sympathetic
nerves intervened. The operations were performed with
a 5 mm angle-free video thoracoscope (Olympus®),
and the flat or horizontal endo-clip was used according
to the anatomical course and position of the sympathetic
nerve (Covidien® Endo Clip Auto Suture™).
All cases were performed using biportal VATS. Incisions were made at the 3rd and 5th intercostal spaces. Carbon dioxide insufflation was not used during videothoracoscopic exploration, as double-lumen intubation provided sufficient exposure. The sympathetic chain was identified through exploration and dissected from the surrounding pleural tissue. Continuity of the sympathetic chain was then interrupted with the application of metallic clips. The inner surface of the corresponding rib was cauterized to prevent conduction through potential alternative pathways (Kuntz nerve). Hemostasis was ensured, free air in the intrathoracic space was aspirated, and incisions were closed without placement of a chest drain after positive pressure ventilation.
Statistical Analysis
IBM® SPSS® Statistics 26.0 was used to analyze the
data and Microsoft® Office™ Excel™ was used to form
graphics. In analyzing the research data, descriptive statistics
(frequency distributions, mean, standard deviation)
were utilized, and the Kolmogorov-Smirnov test was applied
to assess normality distribution. Two-way analysis
of variance (subgroup analysis; Greenhouse-Geisser),
Chi-Square test and T-Test were used for repeated measurements.
The results were evaluated at a 95% confidence
interval and p < 0.05 significance level.
Results
The survey results of 82 patients included in the study were examined. The distribution of the data is in Table 2 and the graphical representation is in Figure 2.Table 2. Satisfaction survey distribution.
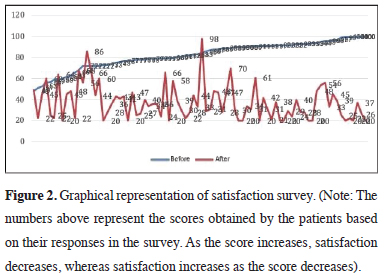 Click Here to Zoom |
Figure 2: Graphical representation of satisfaction survey. (Note: The numbers above represent the scores obtained by the patients based on their responses in the survey. As the score increases, satisfaction decreases, whereas satisfaction increases as the score decreases). |
Group 1 (89%) of 73 euthyroid patients and Group 2 (11%) of 9 patients with subclinical hypothyroidism were statistically compared in terms of hyperhidrosis region, presence of compensatory hyperhidrosis (CH), acceptability of CH and degrees of satisfaction. 16 out of 73 patients in Group 1 were dissatisfied with the surgical outcome, while no patients in Group 2 expressed dissatisfaction. However, this difference was not statistically significant (p = 0.13).
The effect of the survey results on patient groups was investigated by two-way analysis of variance in repeated measurements. The average score of 73 patients in Group 1 before the surgery was 81.86 ± 13.7 and after the surgery it was 37.85 ± 17.03. The average score of 9 patients in Group 2 before the surgery was 86.22 ± 9.35 and after the surgery it was 33.22 ± 11.45. The difference between before and after surgery was statistically significant (Greenhouse-Geisser test; p < 0.0001) however, the effect of patient groups was not significant (Greenhouse-Geisser test; p = 0.27).
Discussion
Sweat glands are primarily regulated by cholinergic innervation [12], which typically stimulates sweat production through acetylcholine release. However, these glands can also respond to adrenergic agents, which trigger sweating through the adrenergic (sympathetic) pathway. This adrenergic stimulation can be blocked by both types of receptor-blocking drugs, specifically by using drugs that inhibit beta (β) receptors, such as propranolol, or alpha (α) receptors, which are part of the sympathetic nervous system. This dual control highlights the complexity of sweat gland regulation under different physiological conditions, such as stress or increased metabolism associated with hyperthyroidism.In hyperthyroidism, hyperhidrosis likely results from an elevated metabolic rate. Excessive sweating and accompanying cardiovascular symptoms are reduced with propranolol administration. However, although propranolol effectively diminishes sweat production triggered by sympathetic activation, it has no effect on individuals without hyperhidrosis or hyperthyroidism when exposed to a hot environment [13].
Our study was based on the hypothesis that, just as overactivity of the thyroid gland can fundamentally affect the thermoregulatory system, underactivity might also disrupt this balance. The results of our research concluded that subclinical hypothyroidism does not influence the outcomes of ETS.
According to Park et al, patients with subclinical hypothyroidism had a higher risk of developing AF in the postoperative period [14]. Kong et al reported that preoperative subclinical hypothyroidism is associated with less favorable cardiovascular outcomes, especially coronary revascularization after bypass surgery [15]. In Comendador et al's study of 467 cases, postoperative atrial fibrillation occurred in 57% of patients with subclinical hypothyroidism versus 30.3% in those without [16]. Blonna et al reported that subclinical hypothyroidism posed a significant risk of dullness following arthroscopic shoulder surgery [17]. Zhao et al found that subclinical hypothyroidism was associated with an increased risk of mortality [18]. Kim et al found that subclinical hypothyroidism had no effect on bone healing [19]. Komatsu et al revealed that hypothyroid patients had slightly longer length of stay in the hospital [20]. Gonzalez-Navarro et al reported that subclinical hypothyroidism was associated with slower postoperative functional recovery in their knee arthroplasty study [21]. Jing et al found that subclinical hypothyroidism increased the incidences of both medical and surgical complications following primary total knee arthroplasty [22]. Kovar et al found that subclinical hypothyroidism could be an independent risk factor for both vascular and overall mortality.
In our study, subclinical hypothyroidism was found not to contribute to the development of atrial fibrillation (AF), nor did it negatively affect postoperative recovery or hospital length of stay. Additionally, subclinical hypothyroidism was not associated with an increased mortality risk or a higher overall complication rate.
When considering other factors affecting sympathectomy, a prospective study by Dias et al examined the relationship between CH, anxiety, depression, and quality of life in patients undergoing thoracoscopic sympathectomy [23]. The study followed 54 patients over 180 days, showing that 93% experienced significant improvements in their quality of life after surgery, although the intensity of CH was strongly correlated with anxiety levels. Despite CH being present in most patients, anxiety did not diminish overall satisfaction with the procedure. In our study, subclinical hypothyroidism was found to have no impact on CH outcomes.
Another key consideration is the anatomical variation in thoracic sympathetic ganglia, as explored by Pei et al [24]. Their research involving 695 patients revealed that anatomical variations, particularly in the third and fourth sympathetic ganglia, influenced both the effectiveness of the surgery and the incidence of CH. While real T3 sympathicotomy was more effective for treating palmar hyperhidrosis, real T4 sympathicotomy was associated with lower rates of moderate-to-severe CH, especially in the chest and back. These findings suggest that preoperative imaging and a customized surgical approach may enhance outcomes by accounting for these anatomical differences. However, in our study, we found that underlying thyroid disorders detected through preoperative TSH evaluations had no effect on surgical outcomes.
Finally, Minqiang et al conducted a randomized controlled trial comparing traditional opioid-based anesthesia with opioid-reduced multimodal anesthesia in patients undergoing thoracoscopic sympathectomy [25]. The study found no significant differences in perioperative complications, postoperative pain levels, or patient satisfaction between the two groups. Similarly, in our study, subclinical thyroid disorders had no effect on these parameters.
Limitations
Although no studies in the literature have evaluated
the relationship between subtly lowered thyroid function
and hyperhidrosis, which was the foundation of our
initial hypothesis for this study, we encountered certain
limitations. According to the ATA/AACE Guidelines
for Hypothyroidism's Adults guideline published by
Garber et al in 2012, subclinical hypothyroidism is defined
as a combination of normal sT4 level and TSH
above the reference limit, but the ongoing discussion
of the TSH reference limit is also mentioned [8]. According
to the said guide, the TSH reference limit was
specified as 4.12 mIU/L by National Center for Health
Statistics (NHANES) III, while it was specified as 2.5
mIU/L according to The National Academy of Clinical
Biochemistry (NACB) data [8]. In our study, we
accepted the upper limit of TSH as 2.5 mIU/L in accordance
with NACB data. We classified TSH values
above this limit as subclinical hypothyroidism. However,
as we mentioned above, there are contradictions
regarding this issue in the literature. Another limitation
is that, due to the retrospective nature of our study and
the relatively small number of patients, we may not
have detected any potential differences between the two
groups. Therefore, we suggest that large, multicenter
studies are needed to further clarify this issue.
In conclusion, our study concluded that subclinical hypothyroidism does not affect the outcomes of endoscopic thoracic sympathectomy. Based on this finding, it can be stated that the presence of subclinical hypothyroidism does not pose a barrier to performing the procedure, nor does it lead to an increased rate of complications. Nevertheless, further research with larger case series is necessary to validate our results. Consequently, our study represents the first of its kind on this topic, and we believe it may serve as an inspiration for future research.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research
and/or authorship of this article.
Ethics approval
The study was approved by The Institutional Ethical
Committee of Yedikule Pulmonology and Thoracic Surgery
Hospital (HNEAH-KAEK 2017/551).
Authors’ contributions
ÖY; designed the study, collected, and analyzed the patient
data, wrote the paper, EÇ; collected the patient data, reviewed
the literature, NY; revised the final version of the
study. All authors read and approved the final manuscript.
Reference
1) Leung AK, Chan PY, Choi MC. Hyperhidrosis. Int J Dermatol
1999; 38: 561-7.
2) Önder M, Aksoy G. Hiperhidroz. Türkderm 2011; 45: 2-9.
3) Apilioğulları B, Bilgiç Ö. Hiperhidroz tedavisi. Genel Tıp Derg
2014; 24: 79-84.
4) Schick CH. Pathophysiology of Hyperhidrosis. Thorac Surg
Clin 2016; 26: 389-93.
5) Garcia Franco CE, Perez-Cajaraville J, Guillen-Grima F, España
A. Prospective study of percutaneous radiofrequency sympathicolysis
in severe hyperhidrosis and facial blushing: Efficacy and
safety findings. Eur J Cardiothorac Surg 2011; 40: 146-51.
6) Macía I, Moya J, Ramos R, Rivas F, Ureña A, Rosado et al.
Primary hyperhidrosis. Current status of surgical treatment. Cir
Esp 2010; 88: 146-51.
7) Lause M, Kamboj A, Fernandez Faith E. Dermatologic manifestations
of endocrine disorders. Transl Pediatr 2017; 6: 300-12.
8) Garber JR, Cobin RH, Gharib H, Hennessey JV, Klein I,
Mechanick JI, et al; American Association of Clinical Endocrinologists
and American Thyroid Association Taskforce on
Hypothyroidism in Adults. Clinical practice guidelines for
hypothyroidism in adults: cosponsored by the American Association
of Clinical Endocrinologists and the American Thyroid
Association. Endocr Pract 2012; 18: 988-1028.
9) Jing W, Long G, Yan Z, Ping Y, Mingsheng T. Subclinical
Hypothyroidism Affects Postoperative Outcome of Patients
Undergoing Total Knee Arthroplasty. Orthop Surg 2021; 13:
932-41.
10) Dias LI, Miranda EC, Toro IF, Mussi RK. Relationship between
anxiety, depression and quality of life with the intensity of reflex
sweating after thoracoscopic sympathectomy for treatment
of primary hyperhidrosis. Rev Col Bras Cir 2016; 43: 354-9.






