2Department of Thoracic Surgery, Karadeniz Technical University Faculty of Medicine, Trabzon, Turkey
3Department of Pulmonology, Recep Tayyip Erdogan University Faculty of Medicine, Rize, Turkey DOI : 10.26663/cts.2024.027
Summary
Esophageal foreign bodies are more common in children than in adults. However, in older individuals without teeth, food swallowed without thorough mastication can get lodged in the esophagus. Herein, we report the case of a 77-year-old woman who presented with severe dyspnea, dysphagia, and a globus sensation in her throat. The patient required intubation owing to progressive dyspnea and rapid peripheral saturation decrease and was found to have a foreign body lodged in her proximal esophagus, which was removed using McGill forceps under direct visualization. Subsequently, the patient was extubated and transferred to the ward. Complaints of dysphagia in older patients with mastication problems should prompt clinicians to consider foreign body impaction. The proximal esophagus is the most common site for foreign body entrapment. If left unmanaged, foreign bodies lodged in the upper gastrointestinal tract can cause serious life-threatening conditions. Appropriate diagnosis and treatment can help minimize potential risks.Introduction
Esophageal foreign bodies (EFBs) are among the most common emergency cases that can be easily treated with complete recovery and no complications via early diagnosis and treatment. The esophagus is the narrowest part of the upper gastrointestinal tract and is the most common site for foreign body entrapment. Foreign body ingestion occurs more frequently in children than in adults [1]. The foreign bodies ingested by adults usually include sharp-edged objects, such as bone fragments, meat with bones, and cartilage, whereas those ingested by children are more likely to include rounded objects, such as metal coins and batteries. Previous studies have reported that food entrapment caused by unchewed food is more common in adults than in children [2]. Herein, we reported the case of a patient who presented to the emergency department (ED) with severe dyspnea, dysphagia, and a globus sensation in her throat due to a piece of red meat lodged in her proximal esophagus.Case Presentation
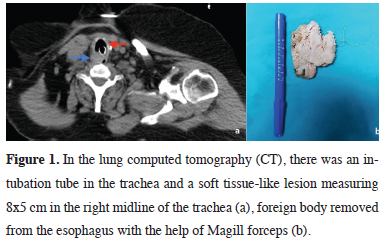
A 77-year-old woman presented to the ED with complaints of coughing, dyspnea, and dysphagia that started while eating. At the time of investigation, the patient was experiencing difficulty in breathing. Patient history collected by the ED physician revealed a suspicion of EFB, prompting the medical team to perform the Heimlich maneuver on the patient. However, this intervention failed to extract any foreign body from the patient’s mouth and led to a gradual decrease in her peripheral saturation to 60% and blue discoloration of her face, requiring rapid intubation. On physical examination after the intubation, the bilateral breath sounds were equal and normal. The patient underwent chest computed tomography (CT), which showed the intubation tube in the trachea and a large lesion resembling soft tissue measuring 8 x 5 cm behind the trachea at the right side of the midline (Figure 1a). The lesion appeared to compress the trachea and shift it forward. After receiving a request for consultation, we performed a clinical examination, reviewed the investigation results, and assessed the oral cavity of the patient with the help of a laryngoscope at bedside in the ED. A foreign body was observed at the site of the esophageal entry and was subsequently extracted using Magill forceps (Figure 1b). Then, esophagoscopy was performed to assess the esophageal lumen, which showed no other foreign bodies. Subsequently, a bronchoscopy was scheduled to rule out the suspicion of a foreign body in the trachea and the patient was extubated. The patient underwent tracheal and main bronchi assessment using a rigid bronchoscope in the ED. On the absence of foreign bodies in the airway, the patient was awakened and transferred to the ward. There was no postoperative complication and the patient was discharged the following day. Written informed consent was obtained from the patient and legally responsible kin of the patient, for publication.
 Click Here to Zoom |
Figure 1: In the lung computed tomography (CT), there was an intubation tube in the trachea and a soft tissue-like lesion measuring 8x5 cm in the right midline of the trachea (a), foreign body removed from the esophagus with the help of Magill forceps (b). |
Discussion
Although EFBs can be encountered in all age groups, they are more frequent in children. However, foreign body ingestion in older individuals is associated with a higher risk of morbidity and mortality [2]. Among foreign body entrapment cases, 87% occurs in the upper esophageal stricture and 13% occurs the middle esophageal stricture, with the lower esophageal stricture being very rarely involved [3]. Most EFBs get lodged at the level of the cricopharyngeus muscle [4]. The most common symptoms associated with EFBs include neck pain, dysphagia, sticking and stinging sensation, hypersalivation, and esophageal obstruction–induced tracheal aspiration [5]. Patient anamnesis is essential for diagnosing EFBs, and its lack can delay the diagnosis [6]. Late diagnosis makes treatment harder and may cause serious and life-threatening complications. Thus, foreign body ingestion requires swift and appropriate diagnosis and treatment [3]. CT helps pinpoint the location of the foreign body and reduce the risk of complications by allowing the removal of the foreign body in a timely manner and is reportedly the preferred imaging modality for the early diagnosis of EFBs [5].As early diagnosis and treatment enables patients to recover without complications and late diagnosis renders treatment more difficult, the first 24 hours are critical, highlighting the importance of prompt measures in EFB cases [5,7]. Missed diagnosis or delay in managing this condition can lead to critical and life-threatening consequences, particularly including esophageal rupture, which can cause mediastinitis, abscess, fistula, empyema, sepsis, and death [8]. Another life-threatening complication, as was observed in our patient, occurs when the foreign body compresses the posterior membranous wall of the trachea, jeopardizing the airway and causing tracheal collapse. This is often caused by a foreign body lodged in the upper esophageal stricture. The Heimlich maneuver, which is one of the methods used when a foreign body obstructs the airway, may also have some undesirable results. The most common complications are rib fractures and pneumomediastinum [9]. We must remember that performing the maneuver incorrectly or using excessive force can have potentially lifethreatening consequences. Foreign bodies closer to the oral cavity are usually easier to remove with the help of instruments such as McGill forceps. However, foreign bodies are more suitable for removal by rigid esophagoscopy, which is carefully performed by experienced physicians under general anesthesia and minimizes the possibility of complications [10].
EFBs are among the most common emergency cases. Foreign bodies entrapped in the upper esophageal stricture can compress the posterior wall of the trachea, causing respiratory failure. In such cases, swift and appropriate diagnosis and treatment can help prevent mortality.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research
and/or authorship of this article.
Authors’ contributions
OT,AB,EST,SK: have given substantial contributions
to the literature search, data collection, study design,
analysis of data, manuscript preparation, analysis interpretation
of the data and review of manuscript, OT,
SK: revised it critically. All authors have participated to
drafting the manuscript, All authors read and approved
the final version of the manuscript.
Reference
1) Kim JK, Kim SS, Kim JI, Kim SW, Yang YS, Cho SH et al.
Management of foreign bodies in the gastrointestinal tract: an
analysis of 104 cases in children. Endoscopy 1999; 31: 302-4.
2) Nandi P, Ong GB. Foreign body in the oesophagus: review of
2394 cases. Br J Surg 1978; 65: 5-9.
3) İnci İ, Özçelik C, Ülkü R, Eren N. Özofagus yabancı cisimleri:
682 olgunun incelenmesi. Turk Gogus Kalp Dama 1999;
7: 148-52.
4) Uyanıkoğlu A, Sert U, Sert H, Cindoğlu Ç. Yaşlı hastalarda servikal
özofagustan yabancı cisim çıkarılması: 2 olgu sunumu.
Endoskopi Gastrointestinal 2015; 23: 89-92.
5) O’Sullivan ST, McGreal GT, Reardon CM, Hehir DJ, Kirwan
WO, Brady MP. Selective endoscopy in management of ingested
foreign bodies of the upper gastrointestinal tract: is it safe?
Int J Clin Pract 1997; 51: 289-92.
6) Chiu YH, Hou SK, Chen SC, How CK, Lam C, Kao WF et al.
Diagnosis and endoscopic management of upper gastrointestinal
foreign bodies. Am J Med Sci 2012; 343: 192-5.
7) Topaloğlu Ö, Akdoğan A, Karapolat S, Türkyılmaz A. A rare
case of esophageal foreign bodies. Turk Gogus Kalp Dama
2022; 30: 136-7.
8) Erbil B, Karaca MA, Aslaner MA, İbrahimov Z, Kunt MM, Akpinar
E, et al. Emergency admissions due to swallowed foreign
bodies in adults. World J Gastroenterol 2013;19: 6447-52.






