2Department of Thoracic Surgery, Denizli State Hospital, Denizli, Turkey DOI : 10.26663/cts.2024.028
Summary
Background: The diagnostic reach of mediastinoscopy depends on adequate tissue sampling. However, adequate tissue sampling may not be possible with conventional blunt dissection methods, especially in the presence of thick encapsulated mediastinal lymph nodes or a mass. It reduces the diagnostic success of mediastinoscopy, and patients may therefore easily result in misdiagnosis. Here, we present a new sharp dissection technique, which we use in cases where adequate tissue sampling from the mediastinal lymph nodes is essential and blunt dissection does not provide it.Materials and Methods: Between 2016-2022, we performed mediastinoscopy in 298 patients and analysed retrospectively. Biopsy could not be taken from mediastinal lymph node and/or mediastinal mass by conventional methods in 26 patients (8.7%). While biopsy could be taken with surgical instruments developed for other operations in 14 of these patients, the needle dissection technique was performed in the remaining 12 patients who cannot be taken a biopsy with conventional and/or surgical instruments developed for other operations.
Results: In patients who needed this technique in mediastinoscopy, all of the tissue with diagnostic value was sampled, no complications were observed, and the most common diagnosis was tuberculosis (n = 8, 66.6%).
Conclusions: The use of surgical instruments developed for other operations such as long and thin aspirator and forceps, endoscopic scissors, injection needle and endoclips in addition to standard surgical instruments in mediastinoscopy and also performing this needle dissection technique may increase the diagnostic success of mediastinoscopy.
Introduction
A variety of techniques are available for a mediastinal nodal and/or mass evaluation including tissue sampling. Mediastinoscopy is an effective method in the investigation of diseases with mediastinal lymphadenopathy or those localized in the mediastinum especially in patients who cannot be diagnosed with noninvasive techniques [1,2]. However, it should be noted that the success of mediastinoscopy is directly correlated to the amount of pathological material harvested. It was indicated that between 2% and 10% of the patients who had a mediastinal disease could not be diagnosed by mediastinoscopy [2]. The factors negatively affecting the success may be the presence of encapsulated mediastinal lymph nodes, therefore sampling can be difficult. Lazzaro and LoCicero stated that endoscopic scissors, endo dissectors and endoclips were additionally used during mediastinal lymph node sampling [3]. When necessary, surgical instruments developed for other operations such as energy devices, endoscopic scissors and forceps supported injection needle can be used through the videomediastinoscope [4]. In this study, we describe a new method in order to increase the amount of tissue harvested which can be used in both video-assisted and conventional mediastinoscopy.Methods
Between 2016-2022, we performed mediastinoscopy in 298 patients who cannot be diagnosed with noninvasive techniques, and analysed retrospectively. The mediastinal lymph node can neither be dissected with aspirators nor sampled with forceps due to the thickness of its capsule is included in the study.
Technique
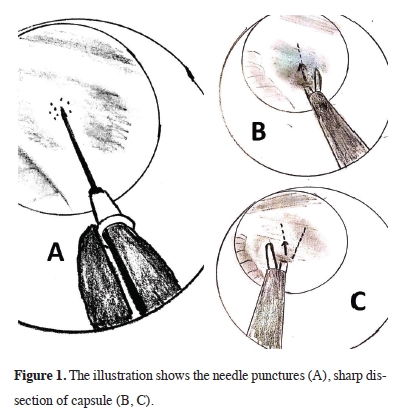
Blunt dissection to lymph nodes with thick capsules
is generally ineffective. Therefore, 5-6 holes are made
with the injection needle placed at the tip of the forceps
in the most suitable part of the capsule for sampling
(Figure 1A). These holes should be drilled in different
places at intervals of about 1 millimeter, thereby weakening
the capsule. Then, the capsule is cut slowly by
making sharp dissection to the weakened capsule with
the lower end of the endoscopic scissors (Figure 1B).
The same procedure is repeated at 30 degrees apical
and the triangular capsule flap is raised (Figure 1C). All
cases were performed by a single surgeon.
 Click Here to Zoom |
Figure 1: The illustration shows the needle punctures (A), sharp dissection of capsule (B, C). |
Results
Biopsy could not be taken from mediastinal lymph node and/or mediastinal mass by conventional method in 26 patients (8.7%). While biopsy could be taken with surgical instruments developed for other operations in 14 of these patients, the needle dissection technique was performed in the remaining 12 patients who cannot be taken a biopsy with conventional and/or surgical instruments developed for other operations. In patients who needed this technique in mediastinoscopy, all of the tissue with diagnostic value was sampled, no complications were observed, and the most common diagnosis was tuberculosis (n = 8, 66.6%). Diagnosis determined using the needle dissection technique shown in table 1.Table 1. Diagnoses determined using the needle dissection technique.
Comment
In many diseases, especially in the differential diagnosis
of granulomatous diseases, a large amount of histological
material may be required. This results in noninvasive
techniques being insufficient for the diagnosis
of granulomatous diseases [5]. Another problem arising
from this situation is that tuberculosis, a type of granulomatous disease, causes technical difficulties in the
operations of some patients. The link between fibrosing
mediastinitis that is thickening of the fibrous tissue in
the mediastinum and tuberculosis has been documented
[6]. This may explain why tuberculous mediastinal
lymphadenitis has a hard capsule. In this respect, the
rigidity of the capsule in benign lesions suggests that it
is a sign of tuberculosis disease, and therefore, this issue
should be further investigated.
It has been stated that 1% of patients could not be diagnosed during mediastinoscopy, and some patients with tuberculosis could actually get wrong diagnosis [7]. The failure to diagnose tuberculosis or the misdiagnosing a potential case of tuberculosis as another disease infers will cause both social and individual problems. If our technique had not been used in these patients, they would have been deprived of treatment, and they would easily be misdiagnosed. Therefore, it can be considered that the use of surgical instruments developed for other operations and this needle dissection technique will increase the diagnostic power of mediastinoscopy. Complications such as massive hemorrhage and hoarseness were not seen in cases where our technique were used, thus, it can be performed safely when it is necessary, with no extra costs incurred.
In conclusion, the use of surgical instruments developed for other operations such as long and thin aspirator and forceps, endoscopic scissors, injection needle and endoclips in addition to standard surgical instruments in mediastinoscopy and also performing this needle dissection technique may increase the diagnostic success of mediastinoscopy.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research
and/or authorship of this article.
Authors' contributions
KK,UK: conceived and designed this study, contributed
to data collection, analyses and interpretation, co-wrote
the study. All authors have read and approved the final
manuscript.
Reference
1) Cheng G, Mahajan A, Oh S, Benzaquen S, Chen A. Endobronchial
ultrasound-guided intranodal forceps biopsy (EBUSIFB)-
technical review. J Thorac Dis 2019; 11: 4049-58.
2) Yazgan S, Ucvet A, Gursoy S, Ceylan KC, Yıldırım Ş. Surgical
Experience of Video-Assisted Mediastinoscopy for Nonlung
Cancer Diseases. Thorac Cardiovasc Surg 2021; 69: 189-93.
3) Lazzaro RS, LoCicero J. Transcervical Mediastinal Lymph Node
Sampling and Lymphadenectomy, Transcervical Mediastinal
Lymph Node Sampling and Lymphadenectomy, General Thoracic
Surgery, 7th Edition, Chapter 169. Eds: Shields TW, LoCicero J;
Reed CE, Feins RH. 2009 Lippincott Williams & Wilkins.
4) Özdemir S, Sönmezoğlu Y, Aydoğmuş Ü, Cansever L, Kocatürk
CI, Bedirhan MA. Is video-assisted mediastinoscopy superior than
standard mediastinoscopy for mediastinal staging of the patients
with lung cancer? Turk Gogus Kalp Dama 2015; 23: 683-9.
5) Onat S, Ates G, Avci A, Yildiz T, Birak A, Akgul Ozmen C,
Ulku R. The role of mediastinoscopy in the diagnosis of nonlung
cancer diseases. Ther Clin Risk Manag 2017; 13: 939-43.






