Summary
Background: Lymphadenopathy occurs due to the proliferation of inflammatory or neoplastic cells within the lymph node or the invasion of the lymph node. Surgical biopsy of supraclavicular lymph nodes in patients with suspected malignancy or lymphadenopathy serves as a valuable tool for determining the treatment plan and cell type. Today, supraclavicular lymph node excision holds an important place in tissue sampling as it is a minimally invasive procedure associated with low morbidity and acceptable diagnostic yield. Moreover, these minimally invasive procedures can be more advantageous as they provide more tissue compared to needle biopsy, with fewer complications.Materials and Methods: In this study, we reviewed our experience with supraclavicular excisional lymph node biopsy in patients suspected of having supraclavicular lymph node metastasis. Detailed medical histories were obtained for all cases, and comprehensive general physical and systemic examinations were performed.
Results: The aim of the study is to evaluate the diagnostic utility, accuracy, and impact on survival of excisional lymph node biopsy in the diagnosis of suspected supraclavicular lymph node metastasis based on histopathological findings. We conclude that excisional biopsy is valuable for accurate diagnosis and appropriate treatment planning when supraclavicular lymph nodes are detected in radiological examinations, even if they are not palpable.
Conclusions: Excisional biopsy is a method that can be safely performed in palpable peripheral lymphadenopathies and does not carry a significant risk of morbidity. It is believed that excisional biopsy of the supraclavicular lymph node has the potential to shorten the time from presentation to diagnosis, thereby saving time and costs in the invasive staging process.
Introduction
Lymphadenopathy occurs due to the proliferation of inflammatory or neoplastic cells within the lymph node or invasion of the lymph node. Surgical biopsy of supraclavicular lymph nodes is a valuable tool for determining the treatment plan and cell type in patients with suspected malignancy or lymphadenopathy. Today, supraclavicular lymph node excision holds a significant place in tissue sampling as a minimally invasive procedure associated with low morbidity and acceptable diagnostic yield. Additionally, these minimally invasive methods are advantageous over needle biopsies as they provide more tissue with fewer complications.The evaluation of supraclavicular lymph nodes plays a crucial role in both diagnosis and determining treatment options. Lymph node biopsies are particularly critical in the diagnosis and staging of metastatic cancer. The primary advantage of supraclavicular lymph node excision is its ability to accurately determine the N stage (regional lymph nodes) in staging. In the TNM staging system for lung cancer, supraclavicular lymph node metastasis is considered N3, and non-surgical approaches or palliative treatments are generally preferred in these cases [1]. The 5-year survival rate for patients with stage IIIB (T0– 4N3M0) non-small cell lung cancer is 15% to 32%. [2].
In this study, we evaluated our clinical experiences with supraclavicular excisional lymph node biopsy in patients with suspected supraclavicular lymph node metastasis. The aim of the study is to assess the diagnostic utility, accuracy, and impact on survival of excisional lymph node biopsy in the diagnosis of suspected supraclavicular lymph node metastasis, in comparison with histopathological findings.
Methods
In our study, patients who underwent supraclavicular lymph node excision biopsy due to suspected supraclavicular lymph node metastasis between 2022 and 2024 were retrospectively evaluated. A total of 50 patients with suspected supraclavicular lymph node metastasis who underwent supraclavicular lymph node excision biopsy were included in the study. Detailed medical histories were obtained for all cases, and comprehensive general physical and systemic examinations were performed. The excised supraclavicular lymph nodes were histopathologically confirmed. In this study, the outcomes of excisional supraclavicular lymph node biopsies performed for diagnostic purposes in our department were analyzed. This study was approved by İnönü University Research Ethical Committee with protocol number 2024/6646.Results
Patients who presented to our clinic with a preliminary diagnosis of malignancy and underwent excisional supraclavicular lymph node biopsy were included in the study. Supraclavicular lymph nodes were identified through palpation and/or imaging methods. Local anesthesia was applied to the skin prior to incision in all patients, and excisional biopsies were completed within an average of 30 minutes. The median interval between preoperative anesthesia preparation and surgery was 3 days (range: 2–5 days). Patients were discharged within an average of 1–3 days in the postoperative period. No complications were observed in any patient during the postoperative period.A total of 50 patients were included in the study, of whom 22 (44%) were female and 28 (56%) were male, with a mean age of 57.8 ± 16.7 years. Among the lymph nodes, 60% were located on the right side, and 40% on the left. The diagnostic distribution was as follows: 28% lymphoma, 44% bronchogenic carcinoma, 24% benign conditions (tuberculosis, toxoplasmosis), and 4% other malignancies (breast cancer, mesothelioma). Of the masses, 50% were palpable and 50% were non-palpable. The mean follow-up period was 13.7 ± 10.2 months, during which 30% of the patients were deceased. Among the masses, 22% were bilateral, and 30% were mobile. Distant metastases were identified in 40% of patients.
According to the anesthesia risk classification, 6% of the patients were ASA I, 52% were ASA II, and 42% were ASA III. While 44% of the patients had no comorbidities, 34% had one comorbidity, and 22% had two comorbidities (Table 1).
Table 1: Demographic and clinical characteristics of the patients
The mortality rate among male patients (42.9%) was significantly higher than that of female patients (13.6%), a difference that was statistically significant (p = 0.025). The mortality rate in patients diagnosed with lymphoma was 35.7%, and for those with bronchogenic carcinoma, it was 45.5%. No mortality was observed in patients with benign or non-bronchogenic malignant conditions. A statistically significant difference in mortality was observed among lymph node pathologies (p = 0.007). The follow-up duration for patients who survived was significantly longer than for those who died (p<0.001). Patients with distant metastases had a significantly higher mortality rate (55%) compared to those without distant metastases (13.3%) (p = 0.002) (Table 2).
Table 2: Comparison of mortality based on patient parameters.
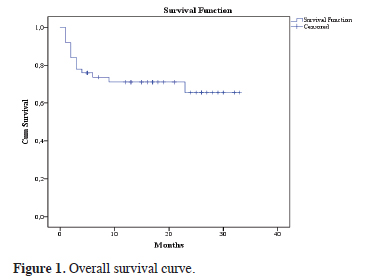
Of the 50 patients included in the study, 15 had died, yielding an overall survival rate of 70%. The mean survival duration for all patients was calculated as 23.8 months. The 3-month, 6-month, 12-month, and 24-month survival rates were 84%, 73.6%, 71.1%, and 65.6%, respectively (Figure 1).
 Click Here to Zoom |
Figure 1: Overall survival curve. |
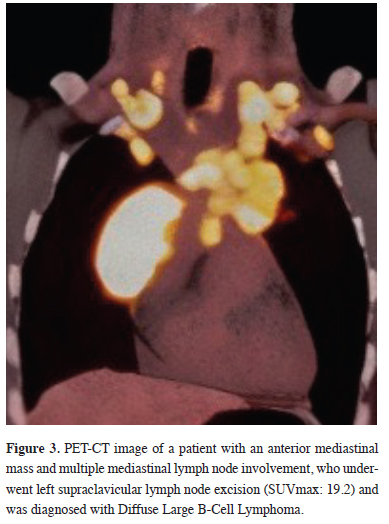
In our study, four patients who underwent surgery with a preliminary diagnosis of malignancy based on positive uptake in PET-CT (positron emission tomography- computed tomography) were diagnosed with tuberculosis. PET-CT of a supraclavicular lymph node (SUVmax 28.7) showing necrotizing granulomatous inflammation, initially misdiagnosed as malignant (Figure 2). In one patient with an anterior mediastinal mass and PET-CT findings showing multiple mediastinal and supraclavicular lymph node involvement, a minimally invasive supraclavicular lymph node excision was performed, and the diagnosis was Diffuse Large B-Cell Lymphoma. The patient was discharged on postoperative day 2 (Figure 3).
 Click Here to Zoom |
Figure 2: PET-CT of a supraclavicular lymph node (SUVmax 28.7) showing necrotizing granulomatous inflammation, initially misdiagnosed as malignant. |
 Click Here to Zoom |
Figure 3: PET-CT image of a patient with an anterior mediastinal mass and multiple mediastinal lymph node involvement, who underwent left supraclavicular lymph node excision (SUVmax: 19.2) and was diagnosed with Diffuse Large B-Cell Lymphoma. |
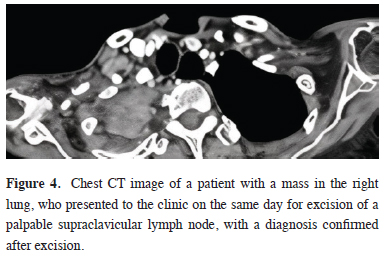
Another patient with a right central mass and pathological- sized supraclavicular lymph node detected on physical examination underwent surgery on the same day of their outpatient clinic visit. The lymph node was excised, and the diagnosis was squamous cell carcinoma (Figure 4).
 Click Here to Zoom |
Figure 4: Chest CT image of a patient with a mass in the right lung, who presented to the clinic on the same day for excision of a palpable supraclavicular lymph node, with a diagnosis confirmed after excision. |
In the majority of cases, the supraclavicular lymph node was completely excised, while in cases with invasion, diagnostic punch biopsies were performed. No complications or mortality were observed in any patient during the postoperative period.
Discussion
Spraclavicular excisional lymph node biopsy significantly contributes to the processes of diagnosis, staging, and determining cell type. Moreover, this method aids in planning advanced investigations, such as molecular- targeted therapy. Additionally, it allows for the avoidance of unnecessary surgical interventions, mor invasive procedures, and potential complications. Although fine-needle aspiration biopsy (FNAB) is a valuable diagnostic tool for distinguishing between benign and malignant lesions, its major disadvantage lies in the inability to obtain sufficient tissue material for diagnosis [3]. Particularly in malignant tumors such as lymphoma, excisional biopsy stands out as a more effective method for accurate identification of subtypes and planning appropriate oncological treatment.Excisional lymph node biopsies should be performed in easily palpable superficial regions such as the axilla, inguinal, or cervical areas. In cases where superficial palpable lymph nodes are not present, biopsies can also be performed from deep lymphadenopathy sites. Lymph nodes larger than 2 cm in diameter typically indicate malignancy or granulomatous diseases [4].
Biopsy is recommended when there is a rapid increase in lymph node size within two weeks, no reduction in size within four to six weeks, or continued growth. During excisional biopsy, it is advised to target the most abnormal-appearing lymph node among those available, even if it is not the most easily accessible [5].
In a study conducted by Darnal et al malignancy was detected in 47% of 273 adult patients who underwent surgical lymph node biopsy. The malignancy rate observed in our study is consistent with the rates reported in this study. On the other hand, in another study by Dorfman et al lymphoma was diagnosed in 40.7% of 118 patients who underwent surgical biopsy. In contrast, Sheresta et al reported that lymphoma was detected in only 7 (5.3%) of 132 patients who underwent excisional lymph node biopsy. These differences are thought to be due to the higher prevalence of tuberculosis lymphadenopathy in endemic regions.
Our clinical experience demonstrates that minimally invasive supraclavicular lymph node biopsies improve diagnostic accuracy while reducing morbidity, particularly for radiologically-detected non-palpable nodes. In our series, we obtained definitive diagnoses in all 25 patients with lymphadenopathy detected solely through imaging, challenging the conventional approach that prioritizes only palpable nodes. The absence of complications confirms the safety of this approach.
PET-CT effectively identifies nodes with increased FDG uptake, aiding biopsy site selection. However, we observed false-positive results in four patients initially misdiagnosed with malignancy but later confirmed to have tuberculosis, reinforcing Werner et al's emphasis on histopathological confirmation [6].
Our malignancy detection rate (74%) exceeds Darnal's reported 47% [7], possibly due to our specialized patient selection criteria. Our lymphoma detection rate (28%) aligns with Metser's findings of 25-30% in scalene node biopsies [8], though lower than Dorfman's 40.7% [9]. Cerfolio demonstrated that these biopsies provide definitive diagnosis in over 90% of cases [10], consistent with our 100% diagnostic accuracy. Our results showed significant survival differences between patients with metastatic disease (55% mortality) versus those without (13.3%), highlighting the prognostic value of accurate assessment.
We recommend excisional biopsy for radiologicallydetected supraclavicular nodes even when non-palpable, supported by Patel's finding that such biopsies yielded sufficient tissue for molecular studies in 94% of cases. While we prefer complete excision of pathological nodes, partial excision may be necessary when nodes are exceptionally large or adherent to critical structures.
In conclusion, supraclavicular lymph node excisional biopsy is safe with minimal morbidity, crucial for definitive diagnosis, and offers a cost-effective solution that shortens time from presentation to diagnosis in the staging process.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research
and/or authorship of this article.
Ethics approval
This study was approved by İnönü University Research
Ethical Committee with protocol number 2024/6646.
Authors’ contribution
MB,MK; made substantial contributions to the design
of the work, made the analysis of data, have drafted the
work, co-wrote and revised it. Both authors read and
approved the final manuscript.
Reference
1) Sihag S. Commentary: Surgery for N3 disease: Next
frontier or has this ship already sailed? J Thorac
Cardiovasc Surg 2019; 158: 1695-7.
2) Faivre-Finn C, Vicente D, Kurata T, Planchard D,
Paz-Ares L, Vansteenkiste JF et al. Four-Year Survival
With Durvalumab After Chemoradiotherapy
in Stage III NSCLC-an Update From the PACIFIC
Trial. J Thorac Oncol 2021; 16: 860-7.
3) Patel JK, Didolkar MS, Pickren JW, Moore RH.
Metastatic pattern of malignant melanoma. J Surg
1978; 35: 807-10.
4) Daniels AC. A method of biopsy useful in diagnosing
certain intrathoracic diseases Dis Chest 1949;
16: 360-6.
5) Mohseni S, Shojaiefard A, Khorgami Z, Alinejad S,
Ghorbani A, Ghafouri A. Peripheral lymphadenopathy:
approach and diagnostic tools Iran J Med Sci
2014; 39: 158-70.
6) Werner L, Keller FA, Bhure U, Roos JE, Tornquist
K, Del Sol Pèrez-Lago M et al. The value of ultrasound-
guided biopsy of fluorodeoxy-glucose positron
emission tomography (FDG-PET)-positive supraclavicular
lymph nodes in patients with suspected
lung cancer. BMC Med Imaging 2017; 17: 41.
7) Darnal HK, Karim N, Kamini K, Angela K. The
profile of lymphadenopathy in adults and children.
Med J Malaysia 2005; 60: 590-8.
8) Metser U, Miller E, Lerman H, Even-Sapir E. Benign
nonphysiologic lesions with increased 18FFDG
uptake on PET/CT: characterization and incidence.
AJR Am J Roentgenol 2007; 189: 1203-10.






