2Department of Thoracic Surgery, Recep Tayyip Erdoğan University Faculty of Medicine, Rize, Tu DOI : 10.26663/cts.2025.003
Summary
Esophageal foreign bodies are emergency cases mostly involving intellectually disabled individuals. An 18-year-old intellectually disabled female patient presented to our clinic complaining about irritability, dysphagia and hypersalivation. Her posteroanterior chest x-ray showed an opacity caused by a safety needle. In her rigid esophagoscopy, a safety needle with an open point was seen, which was localized in the first constriction of her oesophagus. The open sharp point of the safety needle was pulled towards the lumen, held with forceps, bent from its tip towards the clasp, and the pin was removed without any complications. The patient was allowed oral intake of food next day and was discharged without any problems. Esophageal foreign bodies seen in patients with mental retardation may be atypical non-food foreign bodies. Careful endoscopic removal of particularly sharp-pointed objects such as safety needle will prevent complications.Introduction
An esophageal foreign body (EFB) is a clinical entity caused by food or an object swallowed accidentally or intentionally being trapped in the esophagus, which may lead to symptoms such as dysphagia, odynophagia, a prickly sensation and increased secretion. It may result in serious and even life-threatening complications including obstruction in the esophagus, perforation, mediastinitis and sepsis [1]. EFB is more common in adults. Patients with mental retardation (MR) have a special place in the population affected by EFB. These patients tend to swallow non-food objects of various forms.This paper intends to present, also referring to the literature, the diagnosis and treatment stages of a rare esophageal foreign body case involving a patient diagnosed with MR.
Case Presentation
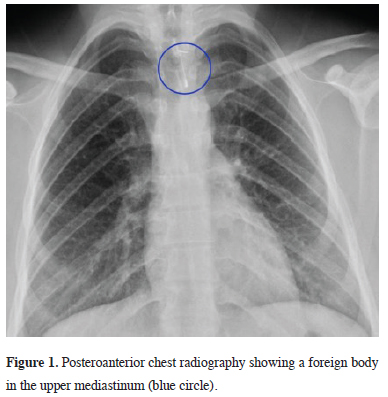
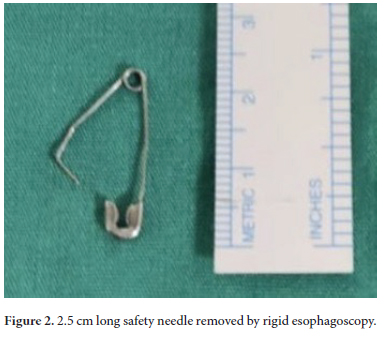
An 18-year-old female patient presented to our clinic with the complaints of irritability, dysphagia and hypersalivation that started a day ago. It was learned that the patient was diagnosed with MR based on the anamnesis taken from her relatives. In her physical examination, her mouth was observed to be full of secretions. Her laboratory tests were normal. In her posteroanterior chest x-ray, a radiopaque appearance of an open safety needle was seen at her superior mediastinum (Figure 1). EFB was considered as an initial diagnosis, and she urgently underwent a rigid esophagoscopy. The esophageal lumen was found normal. An open safety needle with the head part looking down and body part looking up was found in the first constriction of the esophagus. The open sharp point of the safety needle was pulled towards the lumen, held with forceps and bent from its tip. Holding it from its body part with forceps, the safety needle approximately 2.5 cm in length was removed without any complications (Figure 2). The patient was allowed oral intake of food next day and was discharged without any problems. Written informed consent was obtained from the patient or the next of kin for publication.
 Click Here to Zoom |
Figure 1: Posteroanterior chest radiography showing a foreign body in the upper mediastinum (blue circle). |
 Click Here to Zoom |
Figure 2: 2.5 cm long safety needle removed by rigid esophagoscopy. |
Discussion
Cases of EFB commonly occur in the adult population and may lead to significant morbidity and mortality. Patients with special conditions such as MR, psychiatric disorders and those who are demented or edentulous are at higher risk of developing complications associated with an EFB [1]. Due to accompanying eating disorders such as pica and often putting non-food objects into the mouth, atypical foreign bodies in forms different from those seen in normal population can be encountered in patients with MR, such as very lightly chewed foods ingested as a whole, walnuts or hazelnuts with their shells on, soil, stones, wood, paper, metal objects and vinyl gloves [2,3]. In our case, the foreign body was a safety needle, which is actually seen in children most of the time.Individuals with MR are usually unable to express their complaints clearly. To be able to make a correct diagnosis in time and perform early and appropriate treatment, we should consider EFB in the presence of acute symptoms such as swallowing difficulty and hypersalivation in patients with MR and try to discuss the issue with their caregivers in detail to obtain a comprehensive anamnesis. In the present case, we learned from the patient’ mother that the patient has been trying for a long time now to put metal objects into her mouth, they tried to teach her not to do this but have been unable to prevent it. We think that it is important in terms of preventive medicine to inform the relatives of patients with MR about the significance of EFB and its possible complications to prevent recurrent EFBs.
The main purpose of EFB is to remove the foreign body as soon as possible without damaging the surrounding tissues. Otherwise, delayed intervention or late diagnosis complicates treatment and can lead to serious and life-threatening complications [4]. Today, two methods are applied: Flexible and rigid esophagoscopy. While gastroenterologists advocate flexible, surgeons prefer rigid esophagoscopy [5]. Both techniques have advantages and disadvantages, and a common consensus has not emerged for either method [6]. Flexible esophagoscopy also has the advantages of better visualization of the distal esophagus, better overall patient comfort, shorter procedure time, less post-procedural dysphagia, and the ability to perform the procedure with sedation. In rigid esophagoscopy, the advantages include easier access to the proximal esophagus, a larger lumen that allows the use of larger grasping forceps to remove large, irregular and sharp-edged foreign bodies, the ability to remove sharp-edged foreign bodies by taking them into the lumen and causing less trauma to the esophagus and also providing safer airway protection [7]. The complication rate of rigid endoscopy for airway or esophageal FB is low (0.2%-5%) and mortality is rare (<0.1%) [8]. A rigid esophagoscopy under general anaesthesia should be preferred in MR cases for its ease and not requiring patient cooperation [5]. In our patient with mental retardation, we preferred rigid esophagoscopy under general anesthesia because of the possibility of inability to establish effective cooperation during the foreign body removal procedure, the potential for complications due to sudden movements of the patient and to ensure airway safety. An endoscopic removal of a sharp-pointed object such as a safety needle as we encountered in our case requires caution to avoid injury in the mucosa and muscle tissues of the esophagus. Otherwise, potentially mortal complications such as esophageal perforation, abscess, mediastinitis, empyema, fistula formation and sepsis may occur. In our patient, the safety needle was open, and its body part was facing up. Demiroren has already explained in detail in the literature how safety needle in this position can be removed safely [9]. However, in our case, the open piercing tip of the safety needle was stuck in the esophageal mucosa. For this reason, the tip was first pulled to the inner part of the lumen and then bent towards the clasp; the object was held with forceps from its body part and removed safely.
In conclusion, unusual EFBs such as a safety needle may be encountered in patients with MR. The care to be taken during the removal of such sharp-pointed objects by way of rigid esophagoscopy will prevent complications.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contribution
SK,OT,AB: have given substantial contributions to the
literature search, data collection, study design, analysis of
data, manuscript preparation and review of manuscript,
OT, AB: analysis interpretation of the data and review of
manuscript. All authors have participated to drafting the
manuscript, SK,OT: revised it critically. All authors read
and approved the final version of the manuscript. All authors
read and approved the final version of the manuscript.
Reference
1) Garcia I, Varon J, Surani S. Airway Complications from an
Esophageal Foreign Body. Case Rep Pulmonol 2016; 2016:
3403952.
2) Topaloğlu Ö, Akdoğan A, Karapolat S, Türkyılmaz A. A rare
case of esophageal foreign bodies. Turk Gogus Kalp Dama
2022; 30: 136-7.
3) Kamal I, Thompson J, Paquette DM. The hazards of vinyl glove
ingestion in the mentally retarded patient with pica: new implications
for surgical management. Can J Surg 1999; 42: 201-4.
4) Topaloglu O, Buran A, Senturk Topaloglu E, Karapolat S. A rare
reason for intubation: esophageal foreign body lodged in the upper
esophageal stricture. Curr Thorac Surg 2024; 9: 147-9.
5) Topaloglu O, Kılıc Nur K, Karapolat S, Aydın Y, Turkyilmaz A,
Sengul Taslak A et al. Diagnosis, treatment, and management of
esophageal foreign bodies in patients with mental retardation: A
retrospective study from three centers. Turk Gogus Kalp Dama
2024; 32: 179-84.
6) Tsao GJ, Damrose EJ. Complications of esophagoscopy in an
academic training program. Otolaryngol Head Neck Surg 2010;
142: 500-4.
7) Russell R, Lucas A, Johnson J, Yannam G, Griffin R, Beierle E
et al. Extraction of esophageal foreign bodies in children: rigid
versus flexible endoscopy. Pediatr Surg Int 2014; 30: 417-22.






