2Department of Thoracic Surgery, Samsun University, Faculty of Medicine, Samsun, Turkey DOI : 10.26663/cts.2025.004
Summary
Catheter thoracostomy is a common method of pleural effusion; however, complications can occur. This case study describes a rare complication where the catheter extended from the bronchial system into the trachea, with management performed through an endobronchial approach. During catheter thoracostomy, insertion of the catheter under ultrasound guidance at the site of the highest pleural fluid accumulation minimized complications. With hemoptysis, selective bronchial block application with a balloon catheter is a reliable method for treatment.Introduction
Pleural effusion is a common pleural pathology, characterized by symptoms such as shortness of breath and cough. There are more than 50 causes of pleural and systemic diseases [1]. When evaluated based on etiology (e.g., pneumonia, lung cancer, heart failure), pleural effusion may regress following treatment of underlying disease. Where the amount of effusion is excessive, drainage with a pleural drainage catheter or chest tube may be required, depending on the patient’s general condition [2]. Here, we present a case study and the treatment method in which the catheter progressed into the endobronchial system - a very rare complication of catheter thoracostomy.Case Presentation
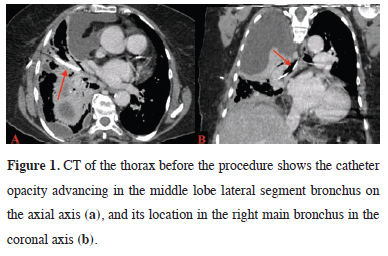
A 66-year-old female patient, who was under oncology follow-up with a diagnosis of endometrial carcinoma, was referred to our Thoracic Surgery Clinic with respiratory distress. Both chest radiography and thoracic computed tomography (CT) detected loculated pleural effusion in the right hemithorax. With the patient in a sitting position, a third-year thoracic surgery resident - under the supervision of a specialist - performed thoracentesis on the patient, who was orthopneic and dyspneic. Thoracentesis was carried out from the right anterior axillary line at the level of the 4th intercostal space. In the presence of serous fluid drainage, catheter thoracostomy was performed using pleuracan® (B. Braun, Melsungen, Germany) from the same area. Hemoptysis developed after the procedure, and air was aspirated through the catheter. Thoracic CT revealed that the catheter extended from the right lung middle lobe lateral segment bronchus to the trachea (Figures 1a,b).
 Click Here to Zoom |
Figure 1: CT of the thorax before the procedure shows the catheter opacity advancing in the middle lobe lateral segment bronchus on the axial axis (a), and its location in the right main bronchus in the coronal axis (b). |
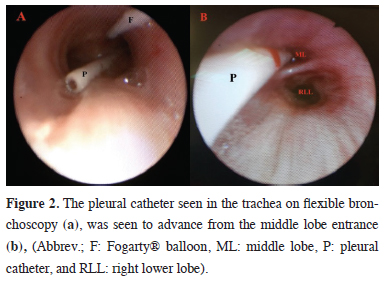
Due to the patient’s hemoptysis, urgent removal of the catheter with bronchoscopy was planned to control the bleeding. Endotracheal intubation was performed under general anesthesia, and during flexible bronchoscopy through the intubation tube, a catheter was inserted into the trachea (Figure 2a). The catheter extended from the trachea toward the middle lobe lateral segment bronchus (Figure 2b). Active bleeding was not observed. However, with the possibility of bleeding after removal of the catheter, closure of the middle lobe entrance was planned with a bronchial blocker. As bronchial blockers could not be obtained under emergency conditions, a 3F Fogarty® balloon (Edwards Lifesciences, CA, USA) was used instead.
 Click Here to Zoom |
Figure 2: The pleural catheter seen in the trachea on flexible bronchoscopy (a), was seen to advance from the middle lobe entrance (b), (Abbrev.; F: Fogarty® balloon, ML: middle lobe, P: pleural catheter, and RLL: right lower lobe). |
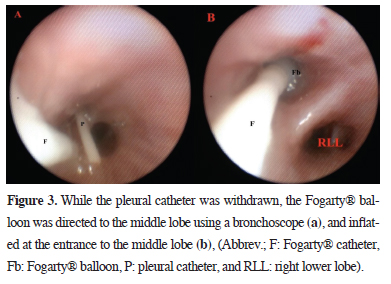
Using a flexible bronchoscope (Karl Storz® 11009BC1, CA, US), the Fogarty® catheter was extended to the lateral segment of the middle lobe, while the catheter was aspirated and retracted in a controlled manner (Figure 3a). The Fogarty® balloon, placed at the entrance of the middle lobe, was inflated (Figure 3b). During the procedure, the patient remained hemodynamically stable, and the Fogarty® balloon was secured within the endotracheal intubation tube. The patient was sedated in the intensive care unit.
 Click Here to Zoom |
Figure 3: While the pleural catheter was withdrawn, the Fogarty® balloon was directed to the middle lobe using a bronchoscope (a), and inflated at the entrance to the middle lobe (b), (Abbrev.; F: Fogarty® catheter, Fb: Fogarty® balloon, P: pleural catheter, and RLL: right lower lobe). |
One day later, under operating room conditions, the middle lobe entrance was visualized through the endotracheal tube using a flexible bronchoscope. The Fogarty® balloon was then removed carefully. There was no blood drainage from the middle lobe lateral segment or other parts of the bronchial system. Therefore, the patient was extubated. The patient did not develop any complications, so a catheter thoracostomy was performed on the right hemithorax under ultrasound guidance two days later. Following pleural fluid drainage and improvement in the patient’s general condition, she was transferred to the oncology department. Written informed consent was obtained from the patient or the next of kin for publication.
Discussion
Catheter thoracostomy can be easily performed under local anesthesia in high amounts of pleural fluid [2]. A pleural drainage catheter is used for this procedure. Pleural drainage catheters are thinner than chest tubes and are placed in the pleural space under the guidance of a trocar. There is a 30% risk of major complications during chest tube and catheter thoracostomy [3]. Therefore, the use of ultrasound guidance is recommended for catheter application [4].This practice, which is integral to residency training in both academic and clinical settings, may result in complications owing to limited opportunities for experience. A study by Kong et al found a significantly higher rate of complications with younger doctors compared with senior doctors [5]. In this study, pleural fluid was accessed during thoracentesis performed by the physician through the appropriate intercostal space. However, advancing the catheter from the locule, where a small amount of fluid was collected, caused it to pass from the lung parenchyma into the bronchial system.
It is very rare for a catheter to reach the bronchial system through the lung parenchyma. A similar complication reported by Kirschbaum et al is the only documented case in the literature [6]. In contrast, the presence of hemoptysis in this patient increased the risk of significant bleeding after pleural catheter removal, so a selective bronchial block was planned to prevent bleeding. Davidson et al recommend the use of a routine bronchial blocker or Fogarty® balloon to isolate bleeding in intubated patients due to the increased risk of major bleeding [7]. Isolation of the injured area with selective bronchial block is important for two reasons. First, it prevents asphyxia by preventing the spread of bleeding to other bronchial systems, and second, it prevents pneumothorax in the pleural space due to parenchymal injury.
This case study demonstrates that placing a pleural catheter at the site of maximum pleural fluid accumulation minimizes the risk of complications. Selective bronchial block with a Fogarty® balloon is a reliable method in cases where hemoptysis develops due to major complications. Furthermore, residency education should prioritize structured training on major complications.
Declaration of Conflicting Interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ Contributions
SG; organized the article and wrote the paper, NGT,AS
contributed to the data collection, SG,NGT,AS; revised
the article. All authors revised the manuscript. The authors
read and approved the final manuscript.
Reference
1) Reuter S, Lindgaard D, Laursen C, Fischer BM, Clementsen
PF, Bodtger U. Computed tomography of the chest in unilateral
pleural effusions: outcome of the British Thoracic Society
guideline. J Thorac Dis 2019; 11: 1336-1346.
2) Reddy CB, DeCamp MM, Diekemper RL, Gould MK, Henry
T, Iyer NP et al. Summary for Clinicians: Clinical Practice
Guideline for Management of Malignant Pleural Effusions.
Ann Am Thorac Soc 2019; 16: 17-21.
3) Haron H, Rashid NA, Dimon MZ, Azmi MH, Sumin JO, Zabir
AF et al. Chest tube injury to left ventricle: complication or
negligence? Ann Thorac Surg 2010; 90: 308-9.
4) Feller-Kopman DJ, Reddy CB, DeCamp MM, Diekemper RL,
Gould MK, Henry T et al. Management of Malignant Pleural
Effusions. An Official ATS/STS/STR Clinical Practice Guideline.
Am J Respir Crit Care Med 2018; 198: 839-49.
5) Kong VY, Oosthuizen GV, Sartorius B, Keene C, Clarke DL.
An audit of the complications of intercostal chest drain insertion
in a high volume trauma service in South Africa. Ann R
Coll Surg Engl 2014; 96: 609-13.






