2Department of Thoracic Pathology, Faculty of Medicine, Suleyman Demirel University, Isparta, Turk DOI : 10.26663/cts.2025.005
Summary
Branchial cleft cysts are common head and neck lesions in children; however, their occurrence in the mediastinum, particularly at lower levels, is extremely rare. When located in the posterior mediastinum, these cysts may cause symptoms such as dysphagia and dyspnea due to compressive effects. Therefore, although uncommon, mediastinal localization should be considered in the differential diagnosis of cystic mediastinal masses.Introduction
Branchial arch anomalies are among the most common congenital lesions of the head and neck region in children [1]. Branchial cleft cysts (BCC) are heterogeneous congenital malformations resulting from incomplete development of the branchial apparatus, which arises from the first four pairs of pharyngeal arches during embryogenesis [2]. While the majority of BCCs are located in the head and neck, mediastinal localization is exceedingly rare. BCCs typically present as cystic lesions or infected cysts; however, in rare instances, they may lead to compressive symptoms such as respiratory distress, chest pain, and dysphagia, particularly when situated in the posterior mediastinum [3]. Herein, we report the case of a 71-year-old patient with a giant BCC located in the subcarinal and postero-inferior mediastinum, presenting with dyspnea, dysphagia, and chest pain. The case is notable for the unusual localization of the cyst and its clinical management.Case Presentation
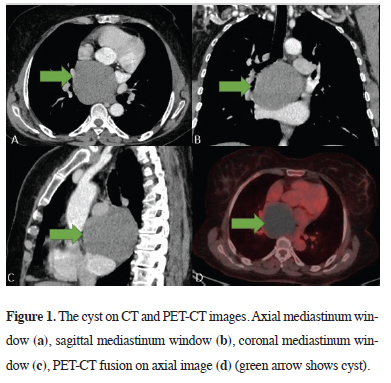
A 71-year-old woman with no comorbidities presented with dysphagia, right-sided chest pain, and shortness of breath for 2 years. The patient was followed up with analgesics and inhaler therapy in another center and no surgical treatment was recommended. It was learned that the lesion was 5 cm when first detected 10 years before she presented to us. Respiratory sounds and vital signs were within normal limits and laboratory tests revealed no abnormality. On direct chest radiography, there was a well-circumscribed opacity in the mediastinum which could be distinguished from the contour of the heart. Thoracic computed tomography (CT) revealed a smoothly circumscribed cystic lesion of approximately 8.5 cm in diameter with a density of 60 Hounsfield units, starting from the subcarinal area and extending inferiorly, adjacent to both main bronchus, esophagus, right pulmonary artery, and vena cava superior (Figures 1a-c). Because of the high density and size of the lesion, positron emission tomography-CT (PETCT) was performed. No increase in metabolic activity was observed (Figure 1d). Endoscopy was performed because of dysphagia to clarify the relationship with the esophagus and seen as normal. The right hemithorax was opened by a posterolateral thoracotomy. In the posterior mediastinum, a cystic structure consisting of vena azygos at the upper border, right inferior pulmonary vein at the lower border, and esophagus, vertebrae, left atrium, right main pulmonary artery, and right main bronchus at the base were detected. The cyst was aspirated with a needle, but couldn’t be drained because of the dense content. Cystotomy was performed and the contents, which were thought to be brown hematoma compatible with pending blood, were drained. The cyst was completely excised. No postoperative complications were observed. Pathologic examination revealed ciliated cylindrical respiratory tract epithelium and lymphoid tissue lining the cyst and the result was interpreted as a BCC (Figure 2). The patient is being followed up smoothly in the postoperative period. The patient was informed in detail about the use of the patient's medical data in academic studies and written consent was obtained from the patient.
 Click Here to Zoom |
Figure 1: The cyst on CT and PET-CT images. Axial mediastinum window (a), sagittal mediastinum window (b), coronal mediastinum window (c), PET-CT fusion on axial image (d) (green arrow shows cyst). |
 Click Here to Zoom |
Figure 2: Histopathological image. Ciliated cylindrical airway epithelium on the cyst surface (a) and lymphoid tissue in the cyst wall (b) (H&E, x40). |
Discussion
The most accepted theory today is that BCC originates from persistent degenerative abnormal branchial arches on the lateral side of the neck [3]. Those located in the mediastinum push the esophagus and trachea and cause difficulty in breathing and swallowing. Thorax CT and a detailed anamnesis are effective in the diagnosis. On thorax CT, it is seen as oval or round masses separated from the surrounding tissues with a smooth border. Endoscopy, barium esophageal radiography, and laryngoscopy should be additionally preferred for BCC [4]. In this case, in addition to the above-mentioned diagnostic methods, we used PET because of the possible risk of malignancy due to advanced age and the high density of the contents.Complete excision with a clean margin after emptying the cyst content is the most preferred method. Open thoracotomy gives surgeons better visibility of cysts and surrounding tissues and a broad region to act in case of complications. On the other hand, VATS is also preferred [2]. We planned surgical treatment without delay because of the absence of an infective clinic and prominent compression symptoms. Due to the size of the cyst and its proximity to the mediastinal main structures, we preferred an open surgical approach, which we thought would be safer in this particular case.
BCC typically consists of ciliated cylindrical epithelium or stratified squamous epithelium with lymphoid tissue and contains lymphoid aggregates. Bronchogenic cysts and esophageal duplication cysts are the most common masses in the posterior mediastinum that require differential diagnosis, but these cysts do not contain lymphoid tissue [5]. BCC generally do not invade the surrounding tissues, are well-circumscribed, and are easy to dissect as in our case. In the literature review, mediastinal localization is rare, while posterior mediastinal localization is even rarer. In terms of size, these cysts usually do not reach extremely large sizes, but in our case, it was much larger than in other cases. We attribute this to the fact that the patient was followed up for a while her treatment was delayed and she was older than the other cases in the literature.
BCC is very rare in the posterior mediastinum and should be differentially diagnosed with other masses. As in our case, surgery is the effective treatment method and the definitive diagnosis is made histopathologically after the use of radiologic imaging methods. As we mentioned, although it is mostly seen in the head-neck region, localization at the subcarinal level and in the postero-inferior mediastinum should be kept in mind.
Declaration of Conflicting Interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ Contributions
RY,SEA: data curation, investigation, methodology,
validation, writing, review and editing, HEY: conceptualization,
data curation, resources, supervision, writing,
review and editing, BK: data curation, investigation.
Reference
1) Adams A, Mankad K, Offiah C, Childs L. Branchial cleft anomalies:
a pictorial review of embryological development and spectrum
of imaging findings. Insights Imaging 2016; 7: 69-76.
2) Ortiz WJ, Ahumada EC, Paz-Moreno OL, McKowen RL, Cervantes
M. Posterior Mediastinal Mass: An Uncommon Presentation
of a Branchial Cleft Cyst. Cureus 2022; 14: e30924.
3) Li LJ, Han ZF, Shang ST. Branchial cleft cyst arising in posterior
mediastinum: A case report. Front Surg 2022; 9: 1088142.






