2Department of Thoracic Surgery, Yüksekova State Hospital, Hakkari, Turkey
3Department of Thoracic Surgery, Çigli Training and Research Hospital, Izmir, Turkey DOI : 10.26663/cts.2025.007
Introduction
Dear Editor,Pneumothorax is a condition characterized by the presence of air between the visceral and parietal pleura, resulting in lung collapse. Collapse may be either partial or complete [1]. The pneumothorax not resulting from trauma or an iatrogenic etiology is known as spontaneous pneumothorax and is categorized as primary and secondary. Secondary spontaneous pneumothorax develops from an underlying pulmonary disease. The etiological factors of secondary spontaneous pneumothorax include diseases such as chronic obstructive pulmonary disease, asthma, interstitial pneumonia, cystic fibrosis, lung cancer, and tuberculosis [2]. The collapse of already impaired lung tissue is a more serious condition for the patient than primary spontaneous pneumothorax. Consequently, secondary spontaneous pneumothorax has been documented in the literature as a more severe and lethal condition [3]. Cases of secondary spontaneous pneumothorax need lung capacity that remains non-functional in respiration due to minimal collapse. Despite the challenges and risks associated with chest tube insertion in these areas, inserting tube thoracostomy with supplementary radiological techniques for localized pneumothorax enhances lung volume contributing respiration, and protects patients from potential outcomes of conservative management, including intubation, critical care, and related complications.
Tube thoracostomy has evolved over time in response to current requirements, both physically and procedurally. Ultrasonography may assist in selecting the intervention site, particularly in the tube thoracostomy performed for fluid drainage [4]. Due to the limited efficacy of ultrasonography in partial pneumothorax, scopy may be utilized in specific patient populations at institutions equipped for such procedures. With the use of a single-plane C-arm fluoroscopy device and realtime imaging support, a dynamic radiographic view can be obtained, closely resembling a moving X-ray. Respiratory- dependent lung movements, the line of an expansion defect, and the real-time visualization of an inserted chest tube can all be observed as if in a video format. This facilitates precise monitoring during the procedure.
When ultrasonography is used, the fact that the probe must be operated by the surgeon limits the ability to perform the intervention bimanually. Alternatively, when handled by another physician, the presence of the ultrasound probe can restrict access to the procedural field, presenting a disadvantage. Furthermore, ultrasound has known limitations in imaging air-containing structures, which may compromise the reliability of the procedure. In computed tomography guided procedures, real-time imaging is not feasible, and stepwise progression using static cross-sectional images interrupts the continuity of the procedure and may reduce its safety. Additionally, the cumulative radiation exposure from each imaging step represents another drawback.
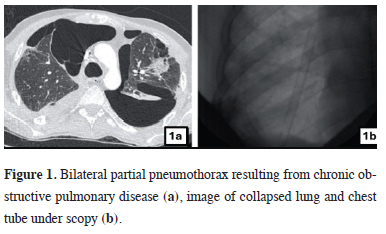
Considering all these limitations, fluoroscopy offers a dynamic version of conventional radiography - a modality frequently utilized and well understood in daily clinical practice. Its ability to provide real-time images significantly enhances procedural safety and precision. Nevertheless, due to the radiation risk, the need for complicated organization, and the potential for time loss, careful selection of cases is necessary. The wellselected patient criteria we recommend should simultaneously include the following: pneumothorax merged from different areas but with separate volumes that are too small for a safe tube thoracostomy, pneumothorax with a total volume causing a decrease in saturation, and secondary spontaneous pneumothorax cases that tube thoracostomy is expected to be beneficial. We have two instances for this procedure which were performed bilateral tube thoracostomy under scopy for bilateral localized secondary spontaneous pneumothorax. The underlying diseases were pneumocystis jiroveci pneumonia related to HIV and chronic obstructive lung disease in these cases. Radiologic images of patients were provided to explain the indications clearly (Figures 1a,b). Subsequent to the procedures, the oxygen requirements decreased in both patients and their follow-ups were conducted in the ward.
 Click Here to Zoom |
Figure 1: Bilateral partial pneumothorax resulting from chronic obstructive pulmonary disease (a), image of collapsed lung and chest tube under scopy (b). |
In cases of secondary spontaneous pneumothorax, scopy may serve as a supplementary technique to tube thoracostomy in well-selected cases that are expected to benefit from tube thoracostomy.
Acknowledgements
We express our gratitude to Associate Professor Ali Özdil
and Professor Ufuk Çağırıcı for their supervision of
the interventions performed in the cases.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research
and/or authorship of this article.
Authors’ contributions
All authors contributed to the study conception and design.
SA, GKÖ, and AKT performed the procedure. SA
wrote the manuscript. GKÖ and AKT collected data. All
authors commented on previous versions of the manuscript.
All authors reviewed and approved the final version
of the manuscript.
Reference
1) Aker C, Onay MS, Cansever L. Pneumothorax and pneumomediastinum
in children. Turk Gogus Kalp Dama 2024; 32(Suppl1):
S37.
2) Gottlieb M, Long B. Managing spontaneous pneumothorax.
Ann Emerg Med 2023; 81: 568-76.






