2Department of Thoracic Surgery, Ondokuz Mayis University, Medical Faculty, Samsun, Turkey
3Department of Thoracic Surgery, Istanbul Atlas University, Medical Faculty, İstanbul, Turkey DOI : 10.26663/cts.2025.010
Summary
Background: Obesity, defined as a body mass index (BMI) of 30 kg/m² or greater, constitutes a substantial global health concern and is associated with an extensive spectrum of comorbid conditions, including numerous malignancies. Among these, lung cancer presents distinctive challenges, particularly with regard to surgical management. The present study examines the impact of obesity on clinical outcomes - namely, prognosis, postoperative complications, and overall survival - among patients undergoing lobectomy for primary lung cancer.Materials and Methods: This retrospective analysis was conducted on a cohort of 1,000 patients who underwent lobectomy for lung cancer between 2010 and 2017. Following the application of predefined inclusion criteria-namely, pathological staging limited to 2A through 3A and the exclusion of cases with concurrent malignancies-a total of 71 patients were deemed eligible for the final analysis. Key clinical and perioperative variables were assessed, including body mass index (BMI), incidence of postoperative complications, duration of hospitalization, operative time, smoking history, and overall survival. Statistical analysis was performed using SPSS version 21.0. Group comparisons were conducted using independent samples t-tests for continuous variables with two categories, while one-way analysis of variance (ANOVA) was applied for comparisons involving more than two groups. Categorical data were evaluated using chisquare tests. A two-tailed p-value of less than 0.05 was considered indicative of statistical significance.
Results: Patients classified as obese exhibited a significantly longer postoperative survival duration when compared to individuals with normal or overweight BMI (p < 0.05). The incidence of postoperative complications was also notably lower in the obese group (p < 0.05). However, no statistically significant differences were observed among the BMI categories in terms of hospital stay length or operative time (p > 0.05). Interestingly, the prevalence of smoking was markedly lower among obese patients (p < 0.001). In contrast, among patients who survived less than five years following surgery, BMI was not found to be significantly associated with either extended hospitalization or postoperative complication rates.
Conclusions: The findings of this study highlight a compelling example of the so-called “obesity paradox” within the context of thoracic surgery. Despite the anticipated risks associated with higher BMI and accompanying comorbidities, obese patients demonstrated more favorable postoperative outcomes and improved survival compared to their non-obese counterparts. These results prompt further investigation into the biological and clinical factors contributing to this paradoxical trend, with the aim of better informing perioperative risk stratification and individualized treatment strategies in lung cancer surgery.
Introduction
Obesity, defined as a body mass index (BMI) of 30 kg/m² or above, is a major public health issue that significantly contributes to the development of cancer and various other pathological conditions. In an increasingly digital and sedentary society, the global prevalence of obesity continues to rise, driven in large part by the widespread availability and consumption of high-calorie, nutrientpoor foods. A 2010 study reported that the prevalence of obesity in the United States had reached 35% [1-3].The burden of obesity becomes particularly evident in the context of complex surgical procedures, such as lung resections, esophageal surgeries, lung transplants, and chest wall reconstructions. These interventions are frequently complicated by intra- and postoperative challenges, including glycemic fluctuations, blood pressure instability, impaired wound healing, deep vein thrombosis, respiratory and systemic infections, ischemic heart disease, renal dysfunction, and cerebrovascular events [4,5].
Despite decades of research, the relationship between obesity and surgical outcomes in thoracic procedures remains a subject of ongoing debate. Clinical experience often suggests increased rates of postoperative complications in obese individuals; however, findings in the literature have been inconsistent. While some studies report a rise in morbidity among obese patients undergoing thoracic surgery, this trend does not appear to extend to mortality rates [6,7].
Interestingly, although obesity is well-documented to increase the risk of overall mortality and is linked to a spectrum of metabolic and clinical disorders, higher BMI has also been associated with improved survival outcomes in certain cancer populations. This apparent contradiction, often referred to as the “obesity paradox,” has prompted further inquiry into the prognostic role of obesity in oncologic surgery. The present study was designed to evaluate the impact of obesity on outcomes following lobectomy in patients with lung cancer.
Methods
This retrospective analysis included a total of 1,000 patients who underwent surgical resection for lung cancer at our institution between 2010 and 2017. Following the application of specific inclusion criteria, 71 patients were selected for detailed evaluation. Eligibility criteria encompassed pathological staging between 2A and 3A, the absence of synchronous malignancies, no prior history of neoadjuvant chemotherapy, absence of concomitant tuberculosis, clear surgical margins confirmed by pathology, availability of all required clinical and laboratory data, and follow-up continuity within our clinic.Preoperative staging involved standard imaging modalities including chest radiography, contrast-enhanced thoracic computed tomography (CT), positron emission tomography-CT (PET-CT), and brain magnetic resonance imaging (MRI). A thorough preoperative work-up was completed for all patients, incorporating pulmonary function testing, complete blood count, comprehensive biochemical profiling, and pre-anesthesia evaluations. Where indicated, patients with coexisting medical conditions were referred to appropriate specialties for further consultation and risk stratification.
Demographic variables - including age, sex, smoking history, and relevant personal and familial health information - were collected from electronic health records and archived patient files. Clinical data such as comorbidities, histological subtype, surgical technique, and operative duration were similarly retrieved. Preoperative height and weight values were extracted from anesthesia assessment forms, and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Based on BMI, patients were stratified into four categories: underweight (<18.5), normal weight (18.5-24.9), overweight (25-29.9), and obese (≥30). Ethical approval for this study was granted by the University Clinical Research Ethics Committee on May 21, 2021 (Reference No. B.30.2.ODM.0.20.08/316).
Statistical Analyses
Statistical analyses were conducted using SPSS software
version 21.0. Descriptive statistics-including means,
standard deviations, and percentages-were reported for
relevant variables. Comparisons between two independent
groups were analyzed using independent samples
t-tests, while comparisons across more than two groups
employed one-way analysis of variance (ANOVA). Relationships
between categorical variables were assessed
using the chi-square test. Survival outcomes were analyzed
using the Kaplan-Meier method, and differences
between groups were compared with the log-rank test.
A p-value below 0.05 was accepted as the threshold for
statistical significance.
Results
The demographic characteristics of the study population are detailed in Table 1. The relationship between body mass index (BMI) and intraoperative variables was first assessed by analyzing surgical duration across BMI categories (Table 2). This analysis did not reveal any statistically significant difference in mean operative time among underweight, normal weight, overweight, and obese patients (p > 0.05).Table 1: Baseline demographic and clinical characteristics of patients undergoing lobectomy.
Similarly, the potential impact of BMI on postoperative length of hospital stay was examined, and no significant variation was found across the different BMI groups (Table 3), with p-values exceeding the threshold for significance (p > 0.05).
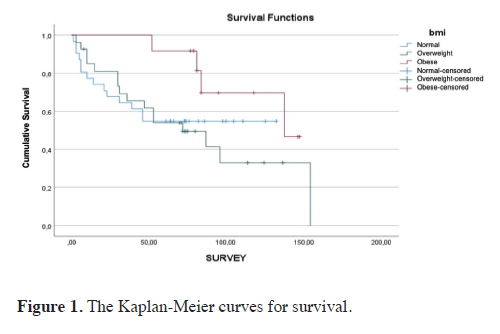
Conversely, a statistically significant difference in median postoperative survival was identified across BMI categories (Table 4), with obese patients demonstrating longer survival than those in the normal and overweight groups (p < 0.05). To further evaluate cumulative survival, a Kaplan-Meier survival analysis was conducted. Although the survival curve appeared more favorable in the obese group, the difference did not reach statistical significance in the log-rank test (p = 0.27). The Kaplan– Meier curves are presented in Figure 1.
 Click Here to Zoom |
Figure 1: The Kaplan-Meier curves for survival. |
Postoperative complication rates were also evaluated in relation to BMI, and the analysis yielded a significant association (p < 0.05). Among patients who did not experience postoperative complications, 27.8% were found to be obese, whereas 51.4% of those who developed complications were categorized as overweight (Table 5).
When assessing the relationship between BMI and prolonged postoperative hospital stay, no statistically significant association was detected (p > 0.05), as presented in Table 6.
Lastly, a strong and statistically significant relationship was observed between BMI and smoking status (Table 7). According to the findings, 52.5% of patients with a normal BMI were active smokers, while 58.3% of non-smokers were classified as obese (p < 0.001).
Discussion
Body mass index (BMI), frequently used as a marker of nutritional status, has long been associated with the pathophysiology of numerous systemic diseases. Obesity and excess weight are established contributors to hypertension and diabetes mellitus, and by extension, to ischemic heart disease and cerebrovascular events [4,8,9]. Lung cancer, the leading cause of cancer-related mortality worldwide, presents a more nuanced picture in this regard. Several epidemiological studies suggest an inverse correlation between BMI and lung cancer incidence [10-12]. This relationship, however, is confounded by smoking - an established carcinogen - that is more prevalent among individuals with lower BMI, complicating interpretation of causality.Cigarette smoking remains the principal risk factor for lung cancer, with reported rates as high as 91.5% [13]. Although the disease may arise from multiple etiologies, the fact that 85-90% of lung cancer cases are linked to smoking highlights its predominant role. Risk intensity correlates with the age of smoking initiation, duration of use, cigarette type, and daily consumption patterns [14].
In our cohort, 83.1% of patients reported current or former smoking, while 16.9% were non-smokers. These results align with findings from Ergün et al [15], who documented a smoking prevalence of 87.3% among lung cancer patients. Although no significant correlation was identified between smoking status and survival in our analysis, a noteworthy observation was the lower prevalence of smoking among obese patients relative to their non-obese counterparts. Given the known contribution of smoking to pulmonary complications following thoracic surgery, the reduced smoking rate among obese individuals may offer a partial explanation for their lower incidence of postoperative complications. The concurrent reduction in smoking prevalence and complication rates in obese patients may reflect a non-random association. Since smoking is a known contributor to postoperative pneumonia, persistent air leakage, and prolonged hospitalization, the protective effect seen in obese individuals may be attributable not solely to body composition but also to diminished tobacco exposure. This potential confounder merits closer examination in future prospective studies with broader inclusion criteria.
Among all patients analyzed, postoperative complications were observed in 49.3%, prolonged hospital stays in 29.6%, and successful recovery in 59.2%. These figures are somewhat lower than those reported in a study by Ülker [16], who found complication rates of 67.5% and 67.3% for conventional and sleeve lobectomy, respectively. That study detailed specific complications, including prolonged air leaks (35.4%), pneumonia (20.7%), reoperation (15.3%), and atrial arrhythmias (11.4%) for conventional lobectomies, while similar distributions were reported for sleeve resections, with arrhythmias (22.4%) and pneumonia (20.9%) being prominent.
In the present analysis, the rate of postoperative complications was significantly lower in the obese group. Although obese patients appeared to have shorter durations of surgery and hospitalization, these differences did not reach statistical significance. This is consistent with prior literature suggesting divergent findings on the role of BMI in surgical risk. Some investigators have identified high BMI as a potential risk factor for cardiopulmonary complications [7,17,18], whereas others argue that these associations are either absent or, in some cases, inversely related [19-21]. Furthermore, some studies suggest that low BMI may be a stronger predictor of adverse outcomes than obesity itself [18,22]. One plausible explanation is that patients with higher BMI are more likely to engage with the healthcare system due to obesity-related comorbidities, thereby enabling earlier cancer detection and improved perioperative optimization.
Regarding postoperative survival, our findings demonstrated significantly longer survival times in the obese cohort compared to the normal and overweight groups. This is in agreement with the meta-analysis by Gupta et al [23], which similarly reported enhanced survival among lung cancer patients with elevated BMI. These observations reinforce the presence of an “obesity-survival paradox” in thoracic surgical oncology.
In our subgroup analysis, a significant relationship was observed between BMI and the occurrence of postoperative complications. Among patients who remained free of complications, 27.8% were obese, whereas 51.4% of those who experienced complications were in the overweight category. While an inverse association was noted between BMI and prolonged hospitalization, this did not reach statistical significance.
Although obesity is widely recognized as a contributor to chronic diseases such as diabetes, hypertension, and coronary artery disease [21,22], its effect on perioperative and postoperative mortality within thoracic surgery remains equivocal. Some studies have identified low BMI as a predictor of worse outcomes, including increased complication rates and reduced survival. Notably, this subset of patients also tends to experience longer operative times. Nevertheless, perioperative mortality remains relatively low across BMI categories. Intriguingly, obese patients tend to experience fewer postoperative complications than those with lower BMI, with lung transplantation being the notable exception. In such cases-particularly among individuals with COPD or cystic fibrosis-elevated BMI correlates with higher perioperative mortality, reinforcing the complexity of this clinical context.
Despite an elevated risk of minor wound infections, obesity has not been conclusively associated with an increase in major complications or mortality [24-27]. In fact, the two largest studies conducted to date on this subject report paradoxical survival advantages in obese patients. In one analysis involving 337 obese lung cancer patients matched 1:1 with non-obese controls, obesity was independently associated with improved survival outcomes [20,21]. Similarly, a large multicenter retrospective study encompassing 18,800 patients who underwent lung resections showed a statistically significant association between higher BMI and reduced 30-day mortality rates [28].
These findings underscore the complexity of interpreting the obesity paradox in surgical outcomes, particularly in thoracic oncology. The apparent survival advantage observed in obese individuals raises questions regarding the interplay of metabolic, immunologic, and behavioral variables that may influence perioperative risk and recovery.
It is important to acknowledge several limitations of this study. The relatively modest sample size restricts the broader applicability of the findings. In addition, the retrospective design limits the ability to establish causal relationships. Furthermore, important covariates such as nutritional status, body composition, and muscle mass were not assessed, which may have influenced outcome measures and introduced residual confounding.
In conclusion, the relationship between obesity and perioperative outcomes in thoracic surgery remains multifaceted and at times contradictory. Although clinical experience might lead one to anticipate increased complication rates among obese patients, emerging evidence points toward a more complex interaction. The survival advantage observed in this study among obese patients undergoing lobectomy and mediastinal lymphadenectomy supports the growing recognition of the obesity paradox in thoracic oncology. Notably, no significant differences were observed in surgical duration or hospital length of stay across BMI groups, and smoking prevalence was lower in the obese population. While these results contribute to the ongoing discourse, the limited sample size and retrospective nature of the analysis highlight the need for large-scale, prospective, multicenter studies to validate these findings and explore the biological mechanisms underlying the observed associations.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Ethics approval
This study was approved by Ondokuz Mayis University
Research Ethics Committee May 21, 2021 (Reference
No. B.30.2.ODM.0.20.08/316).
Authors’ contribution
HK,CI; made substantial contributions to the design
of the work, HK,CI,YBB; made the analysis of data,
HC;CI;YBB; have drafted the work, YBB;AB; revised
it. All authors read and approved the fnal manuscript.
Reference
1) Paul S, Andrews W, Osakwe NC, Port JL, Lee PC, Stiles BM
et al. Perioperative outcomes after lung resection in obese patients.
Thorac Cardiovasc Surg 2015; 63: 544-50.
2) Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence
of obesity and trends in the distribution of body mass index
among US adults, 1999–2010. JAMA 2012; 307: 491-7.
3) Flegal KM, Kit BK, Orpana H, Graubard BI. Association of
all-cause mortality with overweight and obesity using standard
body mass index categories: a systematic review and metaanalysis.
JAMA 2013; 309: 71-82.
4) Prospective Studies Collaboration. Body-mass index and
cause-specific mortality in 900,000 adults: collaborative analyses
of 57 prospective studies. Lancet 2009; 373: 1083-96.
5) Sepesi B, Gold KA, Correa AM, Heymach JV, Vaporciyan AA,
Roszik J et al. The influence of body mass index on overall
survival following surgical resection of non-small cell lung
cancer. J Thorac Oncol 2017; 12: 1280-7.
6) Julien JBS, Aldrich MC, Sheng S, Deppen SA, Burfeind WR
Jr, Putnam JB Jr et al. Obesity increases operating room time
for lobectomy in the Society of Thoracic Surgeons database.
Ann Thorac Surg 2012; 94: 1841-7.
7) Petrella F, Radice D, Borri A, Galetta D, Gasparri R, Solli P et
al. The impact of preoperative body mass index on respiratory
complications after pneumonectomy for non-small cell lung
cancer. Eur J Cardiothorac Surg 2011; 39: 738-44.
8) Manson JE, Colditz GA, Stampfer MJ, Willett WC, Rosner B,
Monson RR et al. A prospective study of obesity and risk of coronary
heart disease in women. N Engl J Med 1990; 322: 882-9.
9) Rexrode KM, Hennekens CH, Willett WC, Colditz GA, Stampfer
MJ, Rich-Edwards JW et al. A prospective study of body
mass index, weight change, and risk of stroke in women.
JAMA 1997; 277: 1539-45.
10) Knekt P, Heliövaara M, Rissanen A, Aromaa A, Seppänen R,
Teppo L et al. Leanness and lung cancer risk. Int J Cancer 1991;
49: 208-13.
11) Kabat GC, Wynder EL. Body mass index and lung cancer risk.
Am J Epidemiol 1992; 135: 769-74.
12) Olson JE, Yang P, Schmitz K, Vierkant RA, Cerhan JR, Sellers TA.
Differential association of body mass index and fat distribution
with three major histologic types of lung cancer: evidence from a
cohort of older women. Am J Epidemiol 2002; 156: 606-15.
13) Göksel T. Akciğer kanserinde risk faktörleri ile histolojik tip
ilişkisi (Türkiye’nin Akciğer Kanseri Haritası Projesi). In: Türk
Toraks Derneği 11. Yıllık Kongresi Bildiri Özetleri Kitabı;
2008; Antalya.
14) Halilçolar H, Tatar D, Ertuğrul G, Çakan A, Acıtaş MG,
Kömürcüoğlu B. Epidemiyoloji. In: Akciğer Kanseri Multidisipliner
Yaklaşım. Ankara: Bilimsel Tıp Yayınevi; 1999. p. 17-22.
15) Ergün D, Savaş İ, Ergün R, Kaya A, Gülhan M. Akciğer kanseri
ve ailesel kanser hikâyesi. Tuberk Toraks 2009; 57: 251-8.
16) Ülker MG. Akciğer kanseri tanısıyla sleeve veya konvansiyonel
lobektomi uygulanan olguların karşılaştırılması: Propensity
skor [specialist thesis]. İstanbul: İstanbul Üniversitesi, İstanbul
Tıp Fakültesi, Göğüs Cerrahisi Anabilim Dalı; 2020.
17) Launer H, Nguyen DV, Cooke DT. National perioperative outcomes
of pulmonary lobectomy for cancer in the obese patient:
a propensity score matched analysis. J Thorac Cardiovasc Surg.
2013;145:1312-8.
18) Thomas PA, Berbis J, Falcoz PE, Le Pimpec-Barthes F, Bernard
A, Jougon J et al. National perioperative outcomes of
pulmonary lobectomy for cancer: the influence of nutritional
status. Eur J Cardiothorac Surg 2014; 45: 652-9.
19) Dhakal B, Eastwood D, Sukumaran S, Hassler G, Tisol W,
Gasparri M, et al. Morbidities of lung cancer surgery in obese
patients. J Thorac Cardiovasc Surg 2013; 146: 379-84.
20) Smith PW, Wang H, Gazoni LM, Shen KR, Daniel TM, Jones
DR. Obesity does not increase complications after anatomic resection
for non-small cell lung cancer. Ann Thorac Surg 2007;
84: 1098-105.
21) Attaran S, McShane J, Whittle I, Poullis M, Shackcloth M. A
propensity-matched comparison of survival after lung resection
in patients with a high versus low body mass index. Eur J Cardiothorac
Surg 2012; 42: 653-8.
22) Jagoe RT, Goodship TH, Gibson GJ. The influence of nutritional
status on complications after operations for lung cancer.
Ann Thorac Surg 2001; 71: 936-43.
23) Gupta A, Majumder K, Arora N, Mayo HG, Singh PP, Beg MS
et al. Premorbid body mass index and mortality in patients with
lung cancer: a systematic review and meta-analysis. Lung Cancer
2016; 102: 49-59.
24) Thomas EJ, Goldman L, Mangione CM, Marcantonio ER,
Cook EF, Ludwig L et al. Body mass index as a correlate of
postoperative complications and resource utilization. Am J
Med 1997; 102: 277-83.
25) lasen J, Junger A, Hartmann B, Jost A, Benson M, Virabjan T,
Hempelmann G. Increased body mass index and peri-operative
risk in patients undergoing non-cardiac surgery. Obes Surg
2004; 14: 275-81.
26) Dindo D, Muller MK, Weber M, Clavien PA. Obesity in general
elective surgery. Lancet 2003; 361: 2032-5.






