Summary
Background: Spontaneous pneumothorax during pregnancy is a rare condition that can pose significant risks to both the mother and the fetus. This report presents the case of a 35-year-old woman with twin pregnancy resulting from in vitro fertilization who developed recurrent pneumothorax on the right side. The patient was initially treated with tube thoracostomy; however, due to prolonged air leakage, video-assisted thoracoscopic surgery with wedge resection was performed. This case underscores the necessity of a multidisciplinary approach for managing pneumothorax during pregnancy and evaluates optimal treatment strategies in light of current literature.Introduction
Spontaneous pneumothorax (SP) during pregnancy represents a highly uncommon clinical entity, with fewer than 100 cases documented in the extant literature [1-3]. In pregnancy, increased oxygen demand, reduced functional residual capacity, and higher intra-abdominal pressure may predispose individuals to SP [2]. Managing SP in pregnancy poses challenges due to the dual concern for maternal and fetal safety. Although mild cases may be adequately addressed through supplemental oxygen therapy and vigilant monitoring, surgical intervention becomes necessary in instances of recurrent or persistent air leakage [3].During pregnancy, elevated progesterone levels act as a respiratory stimulant by increasing the sensitivity of the respiratory center to carbon dioxide, leading to enhanced ventilatory drive. Additionally, progesterone induces bronchodilation by relaxing the smooth muscles of the airways and contributes to mucosal hyperemia and edema, which may cause nasal congestion. These hormonal influences collectively alter pulmonary function during gestation [4].
In twin pregnancies resulting from in vitro fertilization (IVF), respiratory complications are hypothesized to be more frequent due to increased intra-abdominal pressure and hormonal changes. However, the relationship between IVF and pneumothorax remains unclear. This case report discusses the management of recurrent pneumothorax in a twin pregnancy following IVF.
Case Presentation
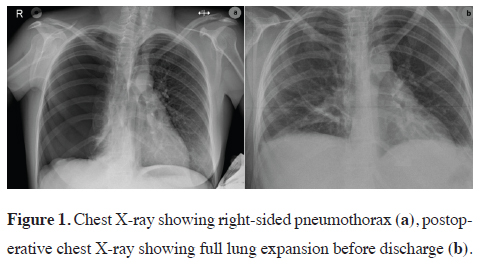
A 35-year-old pregnant woman with twin pregnancy achieved through IVF was admitted to the emergency department during her second trimester with sudden-onset dyspnea. On initial evaluation, the patient’s oxygen saturation was 92% on room air, heart rate was 105 beats per minute, and blood pressure was 129/74 mmHg. Fetal heart rates were confirmed to be normal for both fetuses via bedside ultrasound performed by the obstetrics team. No signs of uterine contractions or vaginal bleeding were noted. She had no history of smoking, underlying lung disease, or trauma. On physical examination, breath sounds were markedly diminished on the right hemithorax. The chest X-ray revealed a right-sided pneumothorax (Figure 1a), and an emergency tube thoracostomy was performed. On the third day of chest tube placement, after 24 hours without air leakage, the chest tube was removed upon confirmation of full lung expansion. The patient was discharged the following day.
 Click Here to Zoom |
Figure 1: Chest X-ray showing right-sided pneumothorax (a), postoperative chest X-ray showing full lung expansion before discharge (b). |
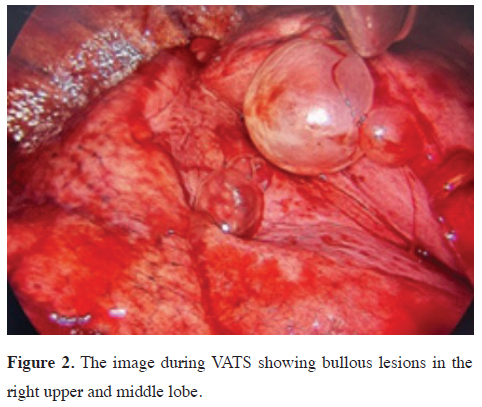
A recurrent pneumothorax was detected on chest X-ray one week after hospital discharge. Tube thoracostomy was performed again. Nevertheless, surgical management was planned due to persistent air leakage and lung expansion failure. Conservative treatment was initially attempted, but due to the failure of lung re-expansion and continued air leakage, it was decided that the conservative treatment should not be extended, considering the risk of infectious and respiratory complications. Bullous structures in the right upper and middle lobes were identified using videoassisted thoracoscopic surgery (VATS) (Figure 2), and wedge resection and pleural abrasion were achieved.
 Click Here to Zoom |
Figure 2: The image during VATS showing bullous lesions in the right upper and middle lobe. |
The postoperative period was uneventful, and no obstetrical complications were observed. During hospitalization, analgesic management was provided with paracetamol, and prophylactic antibiotics were administered according to institutional protocols (cefazolin). No deviations from standard obstetric or thoracic surgical anesthesia protocols were required. The chest tube was removed on the third postoperative day. The control chest X-ray after removal confirmed full lung expansion (Figure 1b). Both infants were delivered healthy with no obstetric or neonatal complications observed. The patient underwent an elective cesarean section under epidural anesthesia. Epidural anesthesia during delivery was chosen to minimize hemodynamic fluctuations and maternal respiratory strain, in accordance with best practices for pregnant patients with prior pulmonary complications. No recurrence or respiratory complications were noted during follow-up. Written informed consent was obtained from the patient for the use of the medical data in academic studies.
Discussion
The patient was monitored by the gynecology and obstetrics department throughout hospitalization, with daily consultations for fetal and maternal assessment and necessary medical adjustments. The obstetric council approved proceeding with pneumothorax surgery. This case highlights the challenges of managing spontaneous pneumothorax during pregnancy and underscores the necessity of a multidisciplinary approach. In this case, a coordinated effort between thoracic surgery, obstetrics, and anesthesiology teams ensured optimal care. Preoperative planning with the anesthesiology team allowed for stable maternal hemodynamics throughout surgery. Simultaneously, the obstetrics team provided daily assessments to monitor fetal development and viability. This collaborative approach enabled effective management of maternal and fetal risks both before and after surgery, contributing to a favorable outcome for both the mother and the fetuses.SP in pregnancy is extremely rare, with fewer than 100 cases reported in the literature [1]. Although pneumothorax is most commonly observed in the third trimester, cases have also been reported in the first and second trimesters [2,3,5]. Risk factors include pre-existing lung diseases, bullous formations, smoking history, respiratory infections, and increased intrathoracic pressure during labor [6]. In this case, a prior history of pneumothorax and the presence of bullous lesions observed in the right upper and middle lobes during surgery are consistent with the known risk factors for spontaneous pneumothorax. Additionally, conditions such as twin pregnancy following IVF may further contribute to pneumothorax development due to increased intra-abdominal pressure and hormonal changes [3,5,6], although the exact mechanism remains unclear.
For the diagnosis of pneumothorax during pregnancy, a maternity lead apron chest X-ray is recommended as the primary imaging modality [3]. Thoracic ultrasound serves as a safe alternative due to its lack of radiation exposure [2]. High-resolution computed tomography (HRCT) may be considered in recurrent cases; however, radiation exposure should be minimized during pregnancy [5]. The chest x ray was obtained after tube insertion, just before chest tube removal and after removal to confirm the lung expansion; and the day after surgery for potential complications. Lead apron was used to shield the fetus. A thorax computed tomography is planned after pregnancy for evaluation of lung parenchyma.
Treatment strategies depend on the pneumothorax size and the patient’s symptoms. In small pneumothoraces (<20%), oxygen support and close monitoring may suffice for asymptomatic patients [6]. Larger pneumothoraces or symptomatic cases require tube thoracostomy [5]. In cases of prolonged air leakage (typically exceeding 5-7 days) or recurrent pneumothorax, surgical intervention becomes necessary [1]. VATS, with wedge resection and pleurodesis, offers significant advantages over open surgery, including less postoperative pain, shorter hospital stays, and lower recurrence rates [2,6]. In this case, VATS was preferred over thoracotomy not only for its minimally invasive advantages but also due to its more favorable hemodynamic profile, which is particularly important during pregnancy.
When planning surgical intervention during pregnancy, maternal and fetal safety should be prioritized. Throughout the patient’s hospital stay, daily fetal monitoring was conducted in collaboration with obstetric specialists. In cases of maternal respiratory failure, cesarean delivery may be considered [3], although spontaneous vaginal delivery is generally deemed safe [5]. Epidural anesthesia may be preferred during delivery to minimize maternal exertion [3]. In this case, the patient delivered via elective cesarean section under epidural anesthesia, which was well tolerated and contributed to maternal-fetal stability. At the time of the initial pneumothorax diagnosis, the patient was at 24 weeks of gestation. Delivery occurred electively at 36 weeks of gestation. Despite the episodes of pneumothorax and surgical intervention, no evidence of preterm labor or intrauterine growth restriction was observed, and fetal development progressed appropriately throughout the pregnancy. No complications arose, eliminating the need for additional interventions.
In conclusion, this case underscores that, although infrequent, spontaneous pneumothorax may arise in twin pregnancies conceived via in vitro fertilization. Expeditious diagnosis, judicious surgical intervention when warranted, and interdisciplinary collaboration are imperative to optimize outcomes for both the mother and the fetuses.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contribution
AK; organized the article and wrote the paper, AK,EZ;
contributed to the data collection, AK,EZ,GÖ; revised
the article. All authors revised the manuscript. The authors
read and approved the final manuscript.
Reference
1) VanWinter JT, Nichols FC 3rd, Pairolero PC, Ney JA, Ogburn
PL Jr. Management of spontaneous pneumothorax during pregnancy:
case report and review of the literature. Mayo Clin Proc
1996; 71: 249-52.
2) Nwaejike N, Aldam P, Pulimood T, Giles R, Brockelsby J, Fuld
J, et al. A case of recurrent spontaneous pneumothorax during
pregnancy treated with video assisted thoracoscopic surgery.
BMJ Case Rep 2012; 2012: bcr0520114282.
3) Akçay O, Uysal A, Samancılar O, Ceylan KC, Sevinc S, Kaya
SO. An unusual emergency condition in pregnancy: pneumothorax.
Case series and review of the literature. Arch Gynecol
Obstet 2013; 287: 391-4.
4) LoMauro A, Aliverti A. Respiratory physiology of pregnancy:
Physiology masterclass. Breathe (Sheff). 2015; 11: 297-301.






