Summary
Schwannomas, also referred to as neurilemmomas, are benign neoplasms arising from Schwann cells within the peripheral nervous system. These tumors may develop at various anatomical sites, including the respiratory system, most commonly involving the chest wall and posterior mediastinum. Primary tracheobronchial schwannomas are exceedingly rare. In this report, we present the case of a 22-year-old male patient with an endotracheal schwannoma originating from the carina and extending into the trachea.Introduction
Schwannomas are well-circumscribed, benign neoplasms originating from Schwann cells in the peripheral nervous system. These tumors are most frequently observed in the mediastinum, retroperitoneum, paraspinal nerve roots, and cerebellopontine angle. Schwannomas located within the endotracheal or endobronchial spaces are exceedingly rare [1]. Due to the atypical clinical presentation and the scarcity of such cases in the literature, we present the case of a 22-year-old male with endotracheal schwannoma arising from the carina and extending into the trachea.Case Presentation
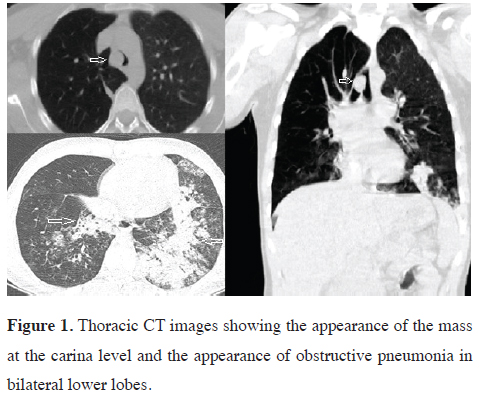
A 22-year-old male patient was referred from an external medical facility with complaints of cough, wheezing, fever, purulent sputum production, and dyspnea. The patient was evaluated upon presentation to the emergency department. Laboratory investigations demonstrated a leukocyte count of 25.87 × 10^9/L, a neutrophil-to-lymphocyte ratio of 93.5, a hemoglobin concentration of 14.6 g/dL, and a platelet count of 361,000/μL, as well as CRP 353. The patient exhibited cyanosis, and arterial blood gas analysis revealed a pH of 7.45, paCO2 of 38 mm Hg, paO2 of 48.5 mm Hg, and sO2 of 84%. Computed tomography of the trachea demonstrated a 15 × 14 mm soft tissue mass extending from the right lateral wall into the lumen of the distal trachea, in addition to localized pneumonic infiltrates in both lower lung lobes (Figure 1).
 Click Here to Zoom |
Figure 1: Thoracic CT images showing the appearance of the mass at the carina level and the appearance of obstructive pneumonia in bilateral lower lobes. |
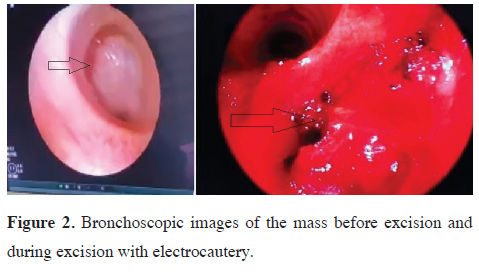
The patient was hospitalized, and antibiotic treatment was initiated due to cyanosis and evidence of infection. Rigid bronchoscopy revealed a mass lesion at the distal end of the trachea, resulting in approximately 80% luminal narrowing. The mass was manipulated using a bronchoscopic cautery aspirator. The lesion was mobile and demonstrated a pedicle originating from the right lateral aspect of the carina. The mass was excised and removed in fragments using forceps. The pedicle of the coagulated lesion was ablated with cautery forceps, and complete luminal patency was achieved to prevent residual tumor tissue. Secretions were aspirated from both bronchial systems. Upon re-examination of the endobronchial site with an optical camera, it was confirmed that the lesion had been completely excised, with no evidence of residual tumor tissue (Figure 2).
 Click Here to Zoom |
Figure 2: Bronchoscopic images of the mass before excision and during excision with electrocautery. |
The patient's cyanosis improved in the early postoperative period, and acute phase reactants decreased rapidly. The patient was discharged with significant recovery of consolidation in the lower lobes on radiologic follow-up. Histopathological examination of the excised tissue confirmed the diagnosis of schwannoma, characterized by spindle-shaped cells arranged in intersecting fascicles, the presence of Antoni A and Antoni B areas, and strong S-100 protein positivity on immunohistochemical staining.
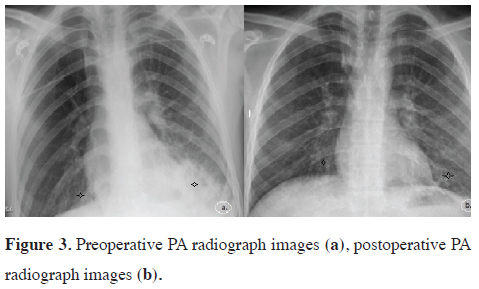
At the fourth-month follow-up after discharge, the patient reported no complications or complaints (Figure 3). Written informed consent was obtained from the patient for the use of the medical data in academic studies.
 Click Here to Zoom |
Figure 3: Preoperative PA radiograph images (a), postoperative PA radiograph images (b). |
Discussion
Schwannomas, also known as neurilemmomas, are benign tumors that develop in the peripheral nervous system from Schwann cells [1]. Schwann cell, named after Theodor Schwann, is a type of glia cell in the peripheral nervous system. Glia cells are in charge of providing support to neurons in the peripheral nervous system. There are two types of Schwann cells: one is in charge of myelination, while the other does not participate in it. The myelin sheath is formed by Schwann cells that wrap around the axons of motor and sensory neurons. Myelin-sheathed nerve fibers allow for rapid transmission of action potentials [2].Schwannomas can occur anywhere in the body, but they are most common in the mediastinum, retroperitoneum, spinal nerve, legs, and cerebellopontine angle. They can be found in the respiratory system, particularly the chest wall and posterior mediastinum. Primary tracheobronchial schwannomas are extremely rare, accounting for 0.2% of all bronchopulmonary tumors, as in our study [1].
The neural structures in the trachea containing Schwann cells are the pulmonary plexus structures with parasympathetic and sympathetic denervation, where Schwannomas develop. The parasympathetic part of this structure is derived from vagus nerve branches, while the sympathetic part is derived from paravertebral sympathetic trunks. The pulmonary plexus is responsible for a variety of functions, including bronchial smooth muscle tone, submucosal glandular mucus secretion, vascular permeability, and blood flow [3].
The first case of bronchial schwannoma was described as a smooth and nodular endobronchial lesion in 1951 [4]. Although it has been reported that primary tracheal schwannomas are observed at a high incidence in adult females of the Asian population, there are also cases reported in childhood and older ages in the literature [1,5].
Although the etiology of schwannomas is unknown, it has been reported that loss and change in the NF2 (neurofibromatosis type 2) gene product of the 22nd chromosome may be related to neurofibromatosis and radiation exposure may play a role in the etiology [2].
Due to their slow growth, most endobronchial schwannomas remain asymptomatic for many years and are usually discovered incidentally during radiological examinations. As in this case, symptomatic patients experience obstruction and obstructive pneumonia symptoms such as cough, hemoptysis, fever, and dyspnea due to the mass obstructing the trachea or main bronchi [6,7].
Tracheobronchial malignant squamous cell carcinomas and adenoid cystic carcinomas are common lesions in the differential diagnosis of endobronchial schwannomas. Carcinoid tumors, malignant fibrosis tumors, rhabdomyosarcomas, hemangioma, laryngotracheal chondroma, granular cell tumors, benign fibrosis tumors, and inflammatory myofibroblastic tumors are also differential diagnoses [1,5,8].
Radiologically, primary endobronchial schwannomas are seen as a sharply circumscribed round, ovoid, or lobule homogenous mass. Thoracic CT examination may reveal the size and location of the mass, as well as whether it has spread outside the lumen [7,8].
Since primary malignant schwannomas are rare and have no specific radiologic or clinical symptoms or findings, it is not possible to predict the exact diagnosis by clinical and radiologic evaluations. However, the histopathologic examination of the tissue obtained by bronchoscopy may provide a definitive diagnosis [2,5,8]. There were radiological interpretations suggesting mucocele or carcinoid tumor in our case. A rigid bronchoscopy excisional biopsy revealed Schwannoma.
Surgery is the gold standard treatment for primary tracheal schwannomas. Surgical treatment options include a wide range of surgical procedures, ranging from sleeve bronchial resection to lung resection, depending on the lesion's location and invasion status, as well as the state of destruction of the distal lung. Similarly, depending on the location of the lesion, whether or not the lesion has a pedicle or not, blood supply, and the presence of co-morbid conditions in the patient, endobronchial treatment modalities should be considered in certain cases. Successful results have been reported in the literature with local radiotherapy applications in cases that cannot be treated surgically or endobronchially [7-9]. Surgery is the gold standard treatment for primary tracheal schwannomas, as emphasized in previous studies on the management of primary tracheal tumors [10]. The lesion in our case was a lesion that almost completely obstructed the trachea at the level of the main carina. Bronchoscopy revealed that the mass grew upwards from a pedicle on the right main bronchial side of the carina to the trachea. It was mobile when touched and provided a lumen opening with its movement. This showed that the patient was breathing. Since the lesion had a pedicle and was mobile, the lesion was firstly coagulated using a cautery aspirator via electrocautery to stop and control the bleeding. It was then excised completely using rigid bronchoscopy forceps. There was no residual tumor in our patient, so no additional intervention or surgical procedure was required. In the third month following the procedure, the patient, whom we closely monitored, had no active complaint.
In conclusion, primary tracheal schwannomas represent rare benign neoplasms of the trachea with a low risk of malignant transformation. This report underscores that endobronchial electrocautery using rigid bronchoscopy, when performed in centers experienced in endobronchial interventions, may constitute a safe and effective therapeutic approach for the management of endobronchial schwannomas.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Author contribution
BM; radiological assesment and radiological image arrangement,
BM,MAE,OT; surgical assesment and detailed
patient information collection, İEÖ; Haematological
assesment, MAT; general consideration and approval
of the whole paper. All authors revised the manuscript.
The authors read and approved the final manuscript.
Reference
1) Lina G, Pengguo H, Zhihua X, Jianxin W, Baoqin B, Mingyue
Z, Junping S. Tracheobronchial schwannoma: a case report and
literature review. J Int Med Res 2023; 51: 3000605221149891.
2) Fallon M, Tadi, P Histology, Schwann Cells. 2023. In Stat-
Pearls. Treasure Island (FL): StatPearls Publishing: 2025.
PMID: 31335036.
3) Gibbins IL. Peripheral autonomic pathways. In The Human
Nervous System, 2nd edn, ed. Paxinos G, Mai JK. Amsterdam,
San Diego, London: Elsevier Academic Press, 2004; pp.
134–189.
4) Straus GD, Guckien JL. Schwannoma of the tracheobronchial
tree. A case report. Ann Otol Rhinol Laryngol 1951; 60: 242–6.
5) Zhang L, Tang W, Hong QS, Lv PF, Jiang KM, Du R. Case
report: A tracheobronchial schwannoma in a child. Respir Med
Case Rep 2020; 30: 101047.
6) Liao H, Song W, Chen N, Chen F, Liu C, Lin F. Left lower lobe
sleeve resection for endobronchial schwannoma. Ann Transl
Med 2019; 7: 50.
7) Lee BR, Choi YD, Kim YI, Lim SC, Kwon YS. Endobronchial
schwannoma treated by rigid bronchoscopy with argon plasma
coagulation. Tuberc Respir Dis (Seoul) 2012; 73: 174-7.
8) Imen T, Sadok BM, Raoudha A, Ksissa S, Yosra B, Yosr BA et
al. Endobronchial schwannoma in adult: A case report. Respir
Med Case Rep 2021; 33: 101396.






