Summary
Schwannomas are slow-growing, encapsulated, benign neoplasms originating from Schwann cells. Although these tumors are frequently asymptomatic, the most commonly reported symptoms include chest pain, back pain, dyspnea, and cough. In this report, we present a case of schwannoma treated surgically at our institution, with particular emphasis on the tumor’s size and the uncommon occurrence of cystic presentation.Introduction
Neurogenic tumors located in the mediastinum originate from embryonic neural crest cells. These tumors are most commonly found in the posterior mediastinum, accounting for 71-95% of cases [1]. They are associated with the sympathetic chain, spinal nerves, or intercostal nerves but can also arise in locations where nerve tissue is present, including intraparenchymal, endotracheal, and chest wall sites [2]. In adults, neurogenic tumors constitute approximately 21% of all mediastinal tumors [3].Schwannomas, a type of neurogenic tumor, originate from Schwann cells and are slow-growing, encapsulated, benign [4]. Although they are typically asymptomatic, schwannomas may present with compression symptoms depending on their location. The most common symptoms include chest and back pain, shortness of breath, and cough [5]. The gold standard treatment for schwannomas is complete excision. In the majority of cases, resection can be successfully performed using thoracoscopic techniques [6].
Herein, we report a case of schwannoma managed surgically at our institution, with particular emphasis on the tumor’s size and the uncommon nature of its cystic presentation.
Case Presentation
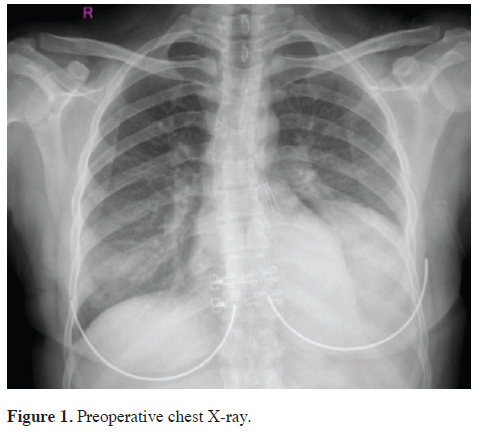
A 37-year-old female patient was admitted to the Department of Thoracic Surgery with the primary complaint of dyspnea. Chest radiography demonstrated increased opacity in the left lower zone with well-circumscribed margins. The preoperative chest radiograph is presented in Figure 1.
 Click Here to Zoom |
Figure 1: Preoperative chest X-ray. |
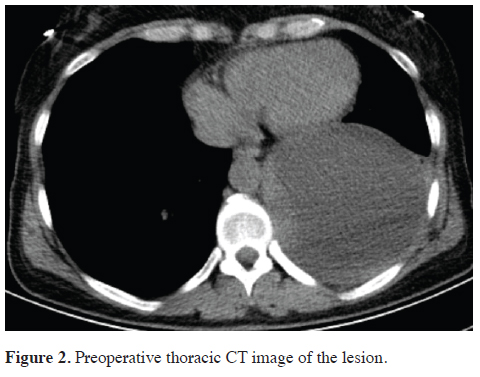
Thoracic computed tomography (CT) demonstrated a cystic, well-circumscribed lesion containing a fluid collection measuring up to 10 cm, located between the pleural layers on the left side. The preoperative thoracic CT image is shown in Figure 2.
 Click Here to Zoom |
Figure 2: Preoperative thoracic CT image of the lesion. |
The patient subsequently underwent exploratory
thoracotomy. Intraoperatively, the lesion was identified
as extrapleural, exerting compressive effects on the diaphragm
and the left lower lobe. The mass, which was
suspected to be neurogenic in origin, was excised in its
entirety along with its capsule (Figure 3).
 Click Here to Zoom |
Figure 3: Intraoperative view of the totally excised cystic lesion. |
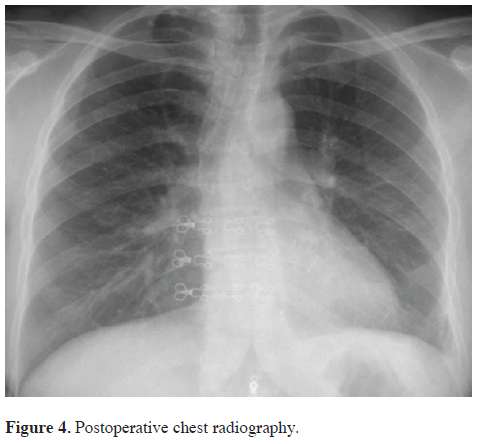
Histopathological examination of the resected specimen confirmed the diagnosis of cystic schwannoma. The postoperative course was uneventful, and the patient was discharged on the fourth postoperative day (Figure 4). Follow-up is ongoing with evaluations at three-month intervals. Written informed consent was obtained from the patient for the use of the medical data in academic studies.
 Click Here to Zoom |
Figure 4: Postoperative chest radiography. |
Discussion
Neurogenic tumors located in the mediastinum originate from embryonic neural crest cells. These tumors are most commonly found in the posterior mediastinum, accounting for 71-95% of cases [1]. In adults, neurogenic tumors account for 21% of all mediastinal tumors [3]. Consistent with this, our case involved a neurogenic tumor located in the posterior mediastinum.Schwannomas typically follow an asymptomatic course. When symptoms occur, they are usually due to compression effects, depending on the tumor’s location. The most common symptoms include chest and back pain, shortness of breath, and cough [5]. In this case, our patient presented with shortness of breath.
Cystic schwannomas are exceptionally rare neurogenic tumors [7]. Contrast-enhanced magnetic resonance imaging (MRI) is the preferred imaging modality for evaluating these tumors and is recommended when suspicion arises [8]. However, in our case, thoracic CT imaging was deemed sufficient preoperatively, and an MRI was not performed.
The differential diagnosis of cystic schwannomas includes other mediastinal tumors, infective diseases such as hydatid cysts and tuberculosis, as well as lung cancer [1]. Preoperative radiological imaging methods and intraoperative surgical exploration play an important role in distinguishing cystic schwannomas from other conditions.
Complete surgical excision remains the gold standard treatment method for these tumors. Recurrence after successful excision is exceedingly rare [9]. In our case, the tumor was successfully treated with total excision.
Video-assisted thoracoscopic surgery (VATS) is a safe and effective approach for the removal of mediastinal tumors. In our case, excision was performed via thoracotomy due to the tumor’s location and size. However, we also consider VATS exploration to be a clinically appropriate option for mediastinal tumors.
In conclusion, cystic schwannomas are rare entities that pose significant diagnostic challenges in the preoperative setting. Complete surgical excision remains the treatment of choice and is associated with favorable outcomes, as demonstrated in the present case.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Author contribution
MAE,EFÇ; radiological assessment and radiological image
arrangement, MAE,OT; surgical assessment and detailed
patient information collection, MHA; general consideration
of the paper. All authors revised the manuscript.
The authors read and approved the final manuscript.
Reference
1) Boland JM, Colby TV, Folpe AL. Intrathoracic peripheral nerve
sheath tumors a clinicopathological study of 75 cases. Human
Pathol 2015; 46: 419-25.
2) Kocatürk C. Mediastinal nörojenik tümörler. Toraks Cerrahisi
Bulteni. 2011; 2: 106-16.
3) Azarow KS, Pearl RH, Zurcher R, Edwards FH, Cohen AJ. Primary
mediastinal masses: a comparison of adult and pediatric
populations. J Thorac Cardiovasc Surg 1993; 106: 67-72.
4) Reynolds M, Shields TW. Benign and Malignant Neurogenic
tumors of the mediastinum in children and adults. General
Thoracic Surgery: Seventh Edition: Wolters Kluwer Health
Adis (ESP); 2011. p. 6422-87.
5) Chu EC-P, Trager RJ. Thoracic schwannoma as an unusual
cause of sciatic pain in the chiropractic office: a case report.
Am J Case Rep 2022; 23: e938448-1.
6) Ishikawa E, Matsumura A, Ishikawa S, Nakamura K, Nose T.
Combined minimally invasive approach using microsurgery and
thoracoscopic surgery for resecting a dumbbell-type thoracic
schwannoma. Minim Invasive Neurosurg 2002; 45: 251-3.
7) Samman A, Bardeesi A, Alzahrani M. Thoracic cystic schwannoma:
case report and review of literature. Spinal Cord Ser
Cases 2021; 7: 7.






