2Department of Thoracic Surgery, Eskisehir City Hospital, Eskişehir, Turkey DOI : 10.26663/cts.2025.017
Summary
Straight back syndrome is an uncommon clinical entity characterized by tracheal compression resulting from loss of the normal dorsal curvature of the thoracic vertebrae and a reduced distance between the manubrium and the thoracic vertebrae. Herein, we present a case in which respiratory distress developed secondary to tracheal compression attributable to straight back syndrome, and partial manubrium sterni resection was performed utilizing a minimally invasive technique.Introduction
The trachea is anatomically situated within the mediastinum, posterior to the sternum. Under normal circumstances, an adequate distance between the trachea and the sternum permits unimpeded tracheal expansion and contraction during respiration. Nevertheless, certain rare chest wall and spinal deformities, traumatic injuries, or malignancies may reduce this distance, resulting in tracheal compression [1,2]. Such compression can lead to airway obstruction and manifest as severe clinical symptoms, including exertional dyspnea, stridor, and, in extreme cases, respiratory failure.Straight back syndrome (SBS), among these anomalies, is a rare clinical entity characterized by loss of the normal dorsal curvature of the thoracic vertebrae and a decreased distance between the manubrium sterni and the thoracic vertebrae [3,4]. These anatomical alterations may result in cardiac manifestations secondary to compression of the heart and great vessels such as cardiac murmurs, mitral valve insufficiency, and pulmonary hypertension or precipitate respiratory complications due to tracheal compression [5].
Tracheal compression secondary to straight back syndrome (SBS) may significantly impair patients' quality of life. Timely diagnosis and the implementation of appropriate therapeutic interventions are essential for alleviating respiratory symptoms attributable to tracheal compression and for preventing associated complications.
This case report describes a patient who developed respiratory distress as a result of tracheal compression secondary to SBS, and who was managed with partial manubrium resection utilizing a minimally invasive approach.
Case Presentation
An 18-year-old female patient presented with a twoyear history of progressively worsening exertional dyspnea. Her medical history was unremarkable for any known comorbidities. The dyspnea was classified as Grade 1 according to the Modified Medical Research Council (mMRC) Dyspnea Scale. Physical examination revealed no appreciable deformities.
Imaging findings
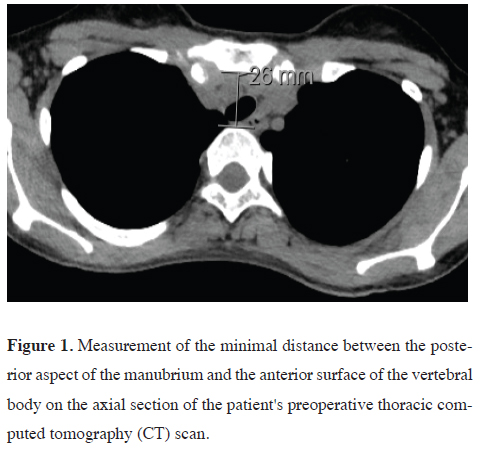
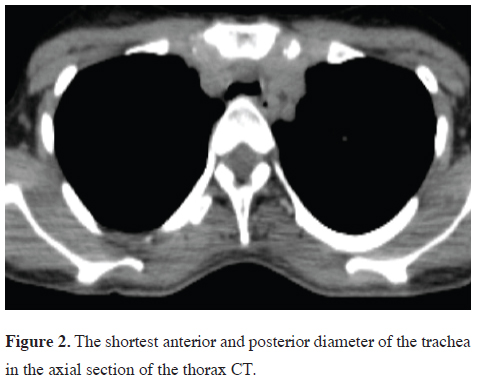
Thoracic computed tomography (CT) revealed that, distal
to the left brachiocephalic artery's origin, the manubrium
produced anterior compression of the trachea,
thereby decreasing the anteroposterior diameter of the trachea. The minimal anteroposterior diameter was
measured at 10 mm, whereas the normative range is 16
to 20 mm. The distance between the posterior cortex of
the manubrium and the anterior surface of the vertebral
body was 26 mm. The manubrium sterni measured 18
mm in thickness and 60 mm in width (Figures 1,2).
 Click Here to Zoom |
Figure 1: Measurement of the minimal distance between the posterior aspect of the manubrium and the anterior surface of the vertebral body on the axial section of the patient's preoperative thoracic computed tomography (CT) scan. |
 Click Here to Zoom |
Figure 2: The shortest anterior and posterior diameter of the trachea in the axial section of the thorax CT. |
Preoperative evaluation
Fiberoptic bronchoscopy revealed compressive narrowing
of the anterior wall starting 2 cm after the tracheal
inlet. However, no tracheomalacia was detected.
Surgical method
With the patient in the supine position, a 3 cm incision
was performed on the manubrium, commencing at the
incisura jugularis. The segment of the manubrium exerting
compression on the trachea was excised utilizing
a V-shaped wedge resection technique (Figure 3). This
intervention alleviated tracheal compression, and the resultant
defect was reinforced with a titanium plate. The
procedure was concluded upon achieving hemostasis.
 Click Here to Zoom |
Figure 3: Operative appearance demonstrating compression of the trachea by the manubrium sterni following V-shaped wedge resection. |
Postoperative course
The patient was extubated postoperatively and mobilized
two hours postoperatively. Marked improvement
in respiratory function was observed promptly.
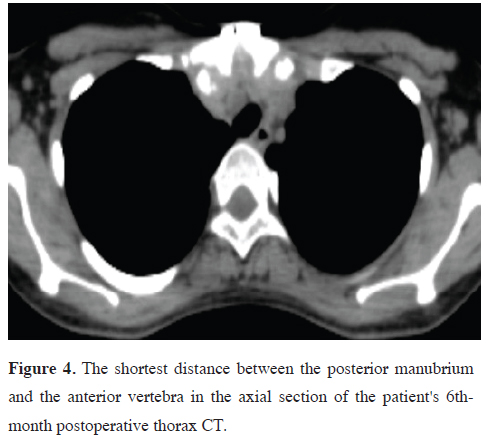
At the six-month follow-up, computed tomography demonstrated resolution of tracheal compression, with a tracheal diameter of 15.2 mm and a manubrium-tovertebral distance of 46–47 mm (Figure 4). Written informed consent was obtained from the patient for the use of medical data in academic research.
 Click Here to Zoom |
Figure 4: The shortest distance between the posterior manubrium and the anterior vertebra in the axial section of the patient's 6thmonth postoperative thorax CT. |
Discussion
In cases of tracheal compression secondary to straight back syndrome (SBS), the primary objective is to achieve adequate decompression by creating sufficient mediastinal space. Surgical interventions may include resection of the posterior manubrium, sternoplasty, correction of concomitant pectus excavatum, or displacement and reconstruction of major vessels contributing to the compression, in order to optimize the available space within the upper mediastinum [5].In a study conducted by Grillo et al, four patients presenting with tracheal compression secondary to SBS were evaluated. Two patients underwent partial manubrial resection in conjunction with re-transposition of the brachiocephalic artery, which was rerouted from the aorta to the right side of the trachea utilizing a graft. Another patient received pectus repair via a modified Ravitch procedure. The remaining patient was managed by placement of a methylmethacrylate plate to preserve the distance between the sternoclavicular joints following partial manubrial resection [6].
Liu et al. reported a case of SBS with tracheal stenosis in which resection of the sternum, costal cartilage, and thymic tissue was undertaken. The resultant chest wall defect was reconstructed, and tracheal compression was alleviated through the application of digitally fabricated material utilizing three-dimensional (3D) technology [7]. In the present case, tracheal compression was similarly attributable to a reduced distance (26 mm) between the posterior aspect of the manubrium and the vertebral bodies. The observation of an abnormally increased transverse diameter of the manubrium indicated that symptomatic relief could be achieved via a less invasive approach, thereby preserving chest wall integrity and avoiding disruption of the sternoclavicular joints. Accordingly, a V-shaped wedge resection of the manubrium was performed. Postoperatively, tracheal compression was effectively resolved. Follow-up computed tomography performed at six months demonstrated an increase in the distance between the posterior surface of the manubrium and the anterior surface of the vertebral bodies to 46-47 mm, as well as an increase in the tracheal anteroposterior diameter to 15.2 mm.
In conclusion, in patients presenting with a decreased anteroposterior thoracic diameter and an increased transverse diameter, tracheal compression should be included in the differential diagnosis of exertional dyspnea. Following early diagnosis and appropriate surgical intervention, significant improvement in respiratory function and quality of life may be achieved. In the present case, tracheal compression was effectively alleviated through a V-shaped wedge resection of the manubrium, utilizing a minimally invasive technique that preserved both patient posture and chest wall integrity. This approach may optimize surgical outcomes and contribute to favorable long-term prognoses.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contribution
VK; organized the article and wrote the paper, EK,FM;
contributed to the data collection, VK,EK,FM; revised
the article. All authors revised the manuscript. The authors
read and approved the final manuscript.
Reference
1) Mi X. Applied Anatomy and Physiology of Trachea, Bronchus
and Esophagus. In: Mu, Z., Fang, J. (eds) Practical Otorhinolaryngology
- Head and Neck Surgery. Springer, Singapore, 2021.
2) Winter RB, Lovell WW, Moe JH. Excessive thoracic lordosis
and loss of pulmonary function in patients with idiopathic scoliosis.
J Bone Joint Surg Am 1975; 57: 972-7.
3) Davies MK, Mackintosh P, Cayton RM, Page AJ, Shiu MF,
Littler WA. The straight back syndrome. Q J Med 1980; 49:
4) Okorozo A, Chiang V, Kim HS, Vimolratana M, Sadoughi A.
A rare case of straight-back syndrome causing airway obstruction.
Respir Med Case Rep 2024; 50: 102024.
5) Schmid S, Schibilsky D, Kalbhenn J, Hassan M, Loop T,
Passlick B et al. Reconstruction of the Mediastinum and Tracheopexy
for Tracheomalacia in Straight Back Syndrome. Ann
Thorac Surg 2021; 112: e41-e44.






