2Department of Thoracic Surgery, Yedikule Chest Diseases and Thoracic Surgery Training and Research Hospital, Istanbul, Türkiye DOI : 10.26663/cts.2025.026
Summary
Background: The aim of this study was to evaluate the prognostic impact of the Geriatric Nutritional Risk Index (GNRI) on survival in patients aged 70 years and older who underwent surgery for earlystage non-small cell lung cancer (NSCLC).Material and Methods: The study included 234 patients with pathological stage 1-2 who underwent surgery at two centers between 2007 and 2020 and who did not receive preoperative neoadjuvant therapy. Patients were divided into two groups based on age: 70-75 years (Group 1) and ≥75 years (Group 2). GNRI was calculated based on serum albumin level and body weight. The difference in survival between the groups was evaluated using Kaplan-Meier analysis, and the prognostic value of GNRI was evaluated using ROC analysis.
Results: No significant association was found between the GNRI value and overall survival (p = 0.506). However, in the ≥75 age group, the survival predictive potential of the GNRI was found to be moderate in ROC analysis (AUC = 0.638). The GNRI cut-off value for this group was determined as 55.7. No significant association was found between the GNRI and clinical parameters such as age, gender, or tumor stage.
Conclusions: The GNRI may be a potential biomarker for predicting survival, especially in NSCLC patients aged 75 and older. Preoperative nutritional support may improve clinical outcomes in patients with low GNRI values. The GNRI may contribute to personalized treatment decisions in the evaluation of elderly NSCLC patients.
Introduction
Non-small cell lung cancer (NSCLC) constitutes approximately 85% of all lung cancers and is often diagnosed at an advanced stage [1]. Surgical resection remains the gold standard treatment for early-stage NSCLC. However, in elderly patients, factors such as diminished immune function, comorbidities, and limited physiological reserve complicate surgical decisionmaking. In recent years, advances in surgical techniques and more rigorous patient selection have rendered surgical treatment increasingly feasible in elderly patients with resectable NSCLC [2-4].The identification of prognostic factors in NSCLC has gained prominence over time. A range of clinical parameters and biomarkers such as hemoglobin, lymphocyte and platelet counts, C-reactive protein (CRP), albumin levels, body mass index (BMI), and nutritional status have been proposed, and various composite indices have been utilized to enhance prognostic accuracy [5-7].
One such index is the Geriatric Nutritional Risk Index (GNRI), developed by Bouillanne et al. in 2005, which has been applied as a prognostic indicator in various malignancies [8,9]. The GNRI, calculated using serum albumin levels and body weight, is clinically valuable as it reflects both the nutritional status and systemic immune response of the patient [10,11]. Nevertheless, current literature lacks sufficient data on the prognostic value of GNRI specifically in elderly NSCLC patients [12].
The objective of this study is to evaluate the prognostic significance of GNRI in patients aged 70 years and older who underwent surgery for early-stage nonsmall cell lung cancer, and to assess its potential utility as a prognostic biomarker.
Methods
This retrospective study was conducted in two thoracic surgery centers between 2007 and 2020, following approval from the institutional ethics committee. The inclusion criteria were as follows: patients aged 70 years or older; those who underwent lung resection and systematic mediastinal lymph node dissection for non-small cell lung cancer (NSCLC); those classified as stage I–II according to the 8th edition of the TNM pathological staging system (T1N0–1M0, T2N0–1M0, T3N0M0); and patients with no history of preoperative neoadjuvant therapy.Exclusion criteria comprised patients with a prior lung resection for indications other than NSCLC, those with locally advanced or metastatic disease (stage III–IV), patients with a history of neoadjuvant therapy, and individuals under the age of 70. A total of 234 patients met the eligibility criteria and were included in the study cohort.
Patients were stratified into two age-based subgroups: Group 1 (70-74 years) and Group 2 (≥75 years). The Geriatric Nutritional Risk Index (GNRI) was calculated using the following formula: GNRI = (1.487 × serum albumin concentration [g/L]) + (41.7 × [actual body weight / ideal body weight]). Ideal body weight was determined using the equation: Ideal body weight = 22 × (height in meters)² (16-19). In cases where the actual body weight exceeded the ideal body weight, the weight ratio was assigned a value of 1.
This study was approved by Ethics Committee of SBU, Dr. Suat Seren Chest Diseases and Thoracic Surgery Training and Research Hospital, (Approval date: 08.10.2025; Number: 2025/64-53).
Statistical Analysis
The distribution of group data was evaluated using the
Shapiro-Wilk test. Depending on data normality, comparisons
between groups were performed using either
the Student’s t- test or the Mann-Whitney U test. Categorical
variables were analyzed using the Chi-square
test. Survival analyses were conducted using Kaplan-
Meier curves and Cox proportional hazards regression.
Receiver Operating Characteristic (ROC) curve analysis and the Youden index were employed to determine the prognostic value and optimal cut-off of the GNRI. All statistical analyses were performed using SPSS version 27.0, and a p-value of <0.05 was considered statistically significant.
Results
Of the total cohort, 176 patients (20 females, 156 males) were aged between 70 and 75 years, while 58 patients (10 females, 48 males) were aged 75 years or older. There was no statistically significant difference between the two groups in terms of gender distribution (p = 0.246). The mean age of Group 1 was 72.1 ± 1.7 years, whereas the mean age of Group 2 was 78.1 ± 2.7 years (Table 1).Table 1. Baseline demographic characteristics of patients according to age group.
Lymphocytosis was found to be significantly lower in patients aged 75 years and above compared to the younger group (p = 0.048). Additionally, lobectomy was performed significantly more frequently in the ≥75 age group (p = 0.011) (Table 2).
Table 2. Comparison of laboratory and physiological parameters between age groups.
No statistically significant differences were observed between the two age groups with respect to the Geriatric Nutritional Risk Index (GNRI), smoking history, hemoglobin levels, C-reactive protein (CRP) levels, pulmonary function parameters, or Charlson comorbidity index scores (Tables 2,3).
Similarly, there were no significant intergroup differences in tumor size, pathological nodal status, TNM stage (9), histopathological subtype, or the surgical approach used (VATS vs. thoracotomy) (Tables 2,3).
Table 3. Comparison of clinicopathological characteristics between age groups.
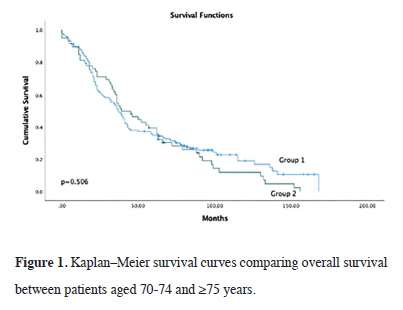
Survival analysis revealed no statistically significant difference in overall survival between the two age groups (p = 0.506). In Group 1 (<75 years), the median overall survival was 59.5 ± 4.3 months (95% CI: 51.0–68.0), while in Group 2 (≥75 years), it was 55.2 ± 5.8 months (95% CI: 43.8–66.5). The median follow-up duration for the entire cohort was 38.0 ± 1.8 months (Table 4, Figure 1).
Table 4. Comparison of survival outcomes between age groups.
 Click Here to Zoom |
Figure 1: Kaplan–Meier survival curves comparing overall survival between patients aged 70-74 and ≥75 years. |
When examining the effect of the geriatric nutritional index value on survival, the area remaining on the ROC curve in the group 75 years of age and older was 63.8% (95% CI: 44.9% - 82.7%). The cut-off value for the geriatric nutritional index in the group 75 years of age and older was 55.7 (Figure 2). GNRI's survival prediction is significant in the ≥75 age group, so the ROC analysis was conducted only in this subgroup.
Discussion
In this study, we investigated the prognostic significance of the Geriatric Nutritional Risk Index (GNRI) in patients aged 70 years and older who underwent surgical resection for early-stage non-small cell lung cancer (NSCLC). ROC curve analysis revealed that the GNRI demonstrated a moderate predictive value for survival in patients aged 75 years and above, with an area under the curve (AUC) of 63.8%. Subgroup analysis identified a GNRI cut-off value of 55.7 in this older age group. These findings suggest that the GNRI may serve as a useful prognostic biomarker in the elderly population, particularly among patients aged 75 years and older.Originally developed as a simple and practical tool to assess malnutrition, the GNRI has gained clinical utility due to its ease of calculation and its reflection of both nutritional and inflammatory status [8-12]. Previous studies have demonstrated the prognostic value of the GNRI in a variety of malignancies, including gastrointestinal cancers, hepatocellular carcinoma, and hematologic malignancies [8-11]. However, data specific to pulmonary malignancies, particularly in elderly cohorts, remain limited. Kinoshita et al previously reported that a low GNRI was associated with poorer survival outcomes in elderly patients with NSCLC, supporting its prognostic relevance in thoracic oncology [12].
Our findings further contribute to the existing literature by demonstrating the potential utility of the GNRI as a prognostic marker in elderly patients undergoing curativeintent surgery for early-stage NSCLC. Nevertheless, it is important to note that the relatively low tumor burden and systemic inflammation typically observed in earlystage disease may limit the prognostic strength of GNRI in this specific patient population. Moreover, the absence of statistically significant associations between GNRI and clinical variables such as age, sex, tumor stage, and histopathological subtype suggests that GNRI may function as an independent prognostic factor in elderly patients.
In surgical patients, poor nutritional status is associated with several adverse postoperative outcomes, including infectious complications, impaired wound healing, and delayed recovery [13,14]. In our study, a significant decrease in GNRI was detected in the over- 75 age group, and its impact on survival was significantly impacted by the ROC curve. Nutrition is becoming increasingly difficult in our country, as it is worldwide, due to socioeconomic factors. This gap is particularly widening in older patients.
Limitations of the study
This study has several limitations. Primarily, its retrospective
and multicenter design may have introduced
variability in data collection and management, limiting
the overall standardization of clinical parameters. In addition,
the sample size, particularly in subgroup analyses,
may not have been sufficient to detect smaller effect sizes.
Prospective studies with larger, more homogeneous
populations are warranted to validate our findings and
further elucidate the prognostic role of GNRI in NSCLC.
Our findings suggest that malnutrition is a prognostic factor in older, early-stage lung cancer. However, due to the observational nature of this study, we were unable to definitively establish the relationship between nutritional status and surveillance. Recently, perioperative nutritional intervention has been recognized as part of a multidisciplinary approach to malnutrition prevention [15]. However, more well-designed prospective studies are needed to determine the impact of preoperative malnutrition treatment on prognosis.
In conclusion, the Geriatric Nutritional Risk Index appears to be a promising prognostic biomarker for elderly patients undergoing surgical treatment for NSCLC. Its predictive value was more pronounced in patients aged 75 years and older. In this context, nutritional interventions, including albumin replacement and dietary supplementation, may be considered in patients with a GNRI below the identified cut-off value of 55.7 prior to surgery. Incorporating the GNRI into preoperative assessment protocols could contribute to more personalized and risk- adapted treatment strategies in elderly NSCLC patients.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research
and/or authorship of this article.
Ethics approval
This study was approved by Ethics Committee of
SBU, Dr. Suat Seren Chest Diseases and Thoracic Surgery
Training and Research Hospital, (Approval date:
08.10.2025; Number: 2025/64-53).
Author contributions
Concept and Design: EYS, GOI, AU; Data Collection:
UC, DK, YT; Analysis and Interpretation: CBS, OS;
Drafting the Manuscript: EYS, GOI; Critical Revision:
AU, CBS.
Reference
1) Jiang S, Yang A, Yang F, Zhu X, Chen X, Li Z et al. The geriatric
nutritional risk index as a prognostic factor in patients
treated with immune checkpoint inhibitors with non-small-cell
lung cancer. J Thorac Dis 2024; 16: 5222-37.
2) Nojiri T, Omura A, Iede K, Katsushima U, Higashiyama M. Clinical
impact of upfront dose reduction of the first cycle of first-line
treatments on safety and survival in elderly patients with nonsmall
cell lung cancer. Asia Pac J Clin Oncol 2025; e14203.
3) Wu GJ, Zhang Y, Liang R, Peng L, Zhang SH. Comparison of survival
outcomes of early-stage non-small-cell lung cancer in elderly
patients (≥ 70 years) treated with stereotactic body radiotherapy
versus surgical resection. World J Surg 2025; 49: 1160-71.
4) Guo Q, He Y, Chen S, Hu S, Wang S, Su L et al. Development
and validation of nomogram for predicting the cancer-specific
survival among patients aged 80 and above with early-stage
non-small cell lung cancer. ANZ J Surg 2025; 95: 106-16.
5) Liu XY, Zhang X, Zhang Q, Ruan GT, Liu T, Xie HL et al.
The value of CRP-albumin lymphocyte index (CALLY index)
as a prognostic biomarker in patients with non-small cell lung
cancer. Support Care Cancer 2023; 31: 533.
6) Liu Q, Xie H, Cheng W, Liu T, Liu C, Zhang H et al. The preoperative
hemoglobin, albumin, lymphocyte, and platelet score
(HALP) as a prognostic indicator in patients with non-small
cell lung cancer. Front Nutr 2024; 11: 1428950.
7) Wei L, Liu C, Wang S, Zhang H, Ruan G, Xie H et al. Sex differences
in the obesity paradox of body compositions in nonsmall
cell lung cancer. Nutrition 2025; 132: 112690.
8) Peng SM, Yu N, Ren JJ, Xu JY, Chen GC, Yang JR et al. The
Geriatric Nutritional Risk Index as a prognostic factor in patients
with advanced non-small-cell lung cancer. Nutr Cancer
2021; 73: 2832-41.
9) Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent
JP, Nicolis I et al. Geriatric Nutritional Risk Index: a new index
for evaluating at-risk elderly medical patients. Am J Clin Nutr
2005; 82: 777-83.
10) Hirabayashi T, Sonehara K, Ozawa R, Hachiya T, Nozawa S,
Agatsuma T et al. Prognostic value of the Geriatric Nutritional
Risk Index in previously untreated patients with advanced nonsmall
cell lung cancer treated with a combination therapy of anti-
PD-1/-PD-L1 antibodies and platinum-based chemotherapy:
a multicenter retrospective study. Oncology 2024; 102: 819-27.
11) Matsuura S, Morikawa K, Ito Y, Kubota T, Ichijo K, Mochizuki
E et al. The Geriatric Nutritional Risk Index and prognostic
nutritional index predict the overall survival of advanced nonsmall
cell lung cancer patients. Nutr Cancer 2022; 74: 1606-13.
12) Kinoshita R, Nakao M, Kiyotoshi H, Sugihara M, Kuriyama
M, Takeda N et al. Geriatric Nutritional Risk Index as prognostic
marker for elderly patients with small cell lung cancer.
Cancer Diagn Progn 2024; 4: 482-8.
13) Lobo DN, Gianotti L, Adiamah A, Adam S, Argiles JM, Bischoff
SC et al. Perioperative nutrition: recommendations from
the ESPEN expert group. Clin Nutr 2020; 39: 3211-27.