Summary
Completion lobectomy is a complex procedure performed mostly in tumor recurrences or after the presence of complications like lobar torsion or bronchopleural fistula. This operation is generally done via re-thoracotomy. Here, we present a case of completion middle lobectomy via videothoracoscopy after an upper lobectomy by thoracotomy.Introduction
Lobectomy via video-assisted thoracoscopic surgery (VATS) is widely performed all around the world with growing experience and better technique. Open surgery is more preferable in completion lobectomy because of adhesions. It is clear that there is a learning curve and VATS lobectomy ratio can be increased with experience [1]. We here in report a case of completion middle lobectomy via (VATS) after an upper lobectomy by thoracotomy in Turkey.Case Presentation
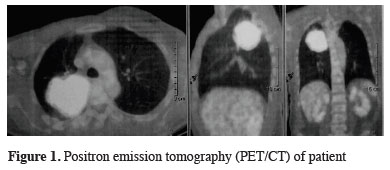
A 50 year-old man presented to our clinic with blood tinged sputum. Thorax computed tomography (CT) showed an 8x7 cm mass in the right upper lobe. The maximum standard uptake value (SUVmax) was 43.5 in positron emission tomography (PET/CT) with no uptake elsewhere (Figure 1).
 Click Here to Zoom |
Figure 1: Positron emission tomography (PET/CT) of patient |
Fiberoptic bronchoscopy revealed an obstruction at the right upper lobe posterior segment ostium with an endobronchial lesion, which was confirmed as an adenocarcinoma. Brain metastasis was excluded with cranial MRI. The patient had no comorbidity and his forced expiratory volume in one second (FEV1) was 2.1 L (89%). Due to the endobronchial localization of the tumor we preferred thoracotomy and a right upper lobectomy was performed after standard cervical mediastinoscopy. At the end of the operation right middle and lower lobes showed full expansion and filled the thoracic cavity. We sutured the middle lobe to the lower lobe because of complete oblique fissure as usual.
On the postoperative day 1, his breath sounds were diminished in the right upper zone. His condition deteriorated, with vital measurement of sinus tachycardia (120 beat/min) and tachypnea (30 breaths/min). Body temperature was 37.8 0C, white blood count was 18,300/mm3 and CRP (C reactive protein) was 12 mg/dL. Blood gas analyses showed; PO2 131 mm/hg, PCO2 47.2 mm/Hg, and pH 7.373 on supplemental oxygen.
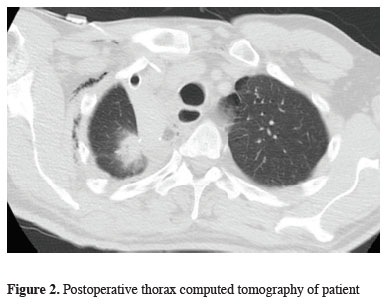
Upon suspicion of a lobar torsion on postoperative chest X-ray and CT (Figure 2) besides clinical findings, rigid bronchoscopy and VATS exploration was planned on the second postoperative day. Rigid bronchoscopic examination showed that right middle lobe bronchus was occluded showing a "fish mouth" appearance.
 Click Here to Zoom |
Figure 2: Postoperative thorax computed tomography of patient |
Under general anesthesia and double lumen endotracheal intubation, he was placed in left lateral decubitus position and VATS exploration using a 10 mm 30 degree rigid endoscope through the former drain incision was performed. As the right middle lobe was congested than, we decided to perform a middle lobectomy. A 4 cm utility incision was made at the fifth intercostal space (Figure 3), the middle lobe vein, artery, bronchus was divided respectively with endostaplers, and the specimen was removed inside an endobag. The patient was discharged on the 4th postoperative day after the second operation uneventfully.
 Click Here to Zoom |
Figure 3: The appearance of the incision after the surgery |
Discussion
Numerous VATS lobectomies have been completed thenceforward the first VATS lobectomy, only now most lobectomies are still completed with thoracotomy. While most lobectomies could be performed with VATS, the lower part is done with this method. Compared with a thoracotomy, VATS offers patients a shorter hospitalization, less pain, and a came around, not to compromise on operational adequacy [1,2]. VATS lobectomy is performed increasingly for early-stage lung cancer. Several published reports thoracoscopic lobectomy can be performed safely and has satisfactory oncologic results [3].Lobar torsion may occur spontaneously, due to blunt trauma or as a postoperative complication of thoracotomy with or without lung resection [4]. Physical findings consist of fever, tachycardia, sudden termination of air leak and reduction of breath sounds at the affected lung field. The radiologic finding is rapid opacification of the affected lobe [4,5].
Postoperative lobar torsion is an infrequent, however it is a life-threatening complication. Several previous cases have been treated with completion lobectomy. When preserving a twisted lobe, it is important to consider the damage to the twisted lung, risk of thrombosis, and residual pulmonary function [6].
In the literature, right upper lobe resections is reported as the most common cause of the lobar torsion, whereas the second most common cause is resection of the left upper lobe [5]. Middle lobe torsion rate is reported as 0.089-0.3%. The management is generally done via exploration on thoracotomy with the resection of the affected lobe [7]. Lobar torsion after pulmonary resection has a low incidence and a nonspecific presentation. When lobe torsion is suspected reoperation and pulmonary resection should be performed to minimize mortality, similar to the management we performed in this case [5].
Completion lobectomy is speculated that it requires dissection of dense adhesions and thus results in prolonged operative time, excusive blood loss, and increased morbidity [8]. However, in such cases requiring prompt surgical intervention for postoperative complication, VATS may be feasible, and can be the first option of choice. The most common cause of conversion to open thoracotomy in VATS lobectomy is adhesions, which is reduced with increasing experience. In the early post-operative period we can use thoracoscopic surgery owing to less adhesions.
As a conclusion, we suggest that in similar cases, VATS must be tried or even forced to be completed if a complication due to the first resection is faced.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Cosgun T, Baysungur V, Tezel C, Okur E, Alpay L, Kutlu CA et al. Learning and improvement process of video-assisted thoracoscopic lobectomy: experiences of Süreyyapaşa. Turk Gogus Kalp Dama 2014; 22: 589-95.
2) McKenna Jr, Houk WV. New approaches to the minimally invasive treatment of lung cancer. Curr Opin Pulm Med. 2005; 11: 282-6.
3) Shaw JP, Dembitzer FR, Wisnivesky JP, Litle VR, Weiser TS, Yun J, et al. Video-assisted thoracoscopic lobectomy: state of the art and future directions. Ann Thorac Surg. 2008; 85: 705-9.
4) Kanemitsu S, Tanaka K, Suzuki H, Tokui T, Kinoshita T. Pulmonary torsion following right upper lobectomy. Ann thorac cardiovasc surg. 2006; 12: 417-9
5) Cable DG, Deschamps C, Allen MS, Miller DL, Nichols FC, Trastek VF et al. Lobar torsion after pulmonary resection: Presentation and outcome. J Thorac Cardiovasc Surg 2001; 122: 1091-3
6) Sakai M, Kurimori K, Saeki Y, Kitazawa S, Kobayashi K, Iguchi K, et al. Video-assisted thoracoscopic conservative repair of postoperative lobar torsion. Ann Thorac Surg 2014; 98: 119-21.






