

Summary
Background: The preferred site of venous access ranges from deep veins (internal jugular or subclavian veins) to superficial veins (external jugular, anterior jugular, and upper limb veins). The aim of the study is to evaluate experience of single surgeon and compare the outcomes of the subclavian (SCV), internal jugular (IJV), and external jugular (EJV) veins in terms of procedure time and complications retrospectively.Materials and Methods: The study included 327 patients who had port placement between 2012 and 2018. The mean age of all cases was 55.67 years, and the patients were divided into 3 groups according to venous sites; subclavian (SCV), internal jugular (IJV), and external jugular veins (EJV). Only local anesthesia was given and no antibiotic prophylaxis was provided before the intervention. The 3 groups were compared regarding age, sex, primary tumor site, procedure time, and complications.
Results: The procedure was significantly longer in the SCV group than the other 2 (43.35 min vs 34.58 and 33.71 min). Removal of the catheter was less common in the IJV group than the other 2 groups. Overall complications in the IJV group were lower than the other 2 groups, especially catheter malposition and pneumothorax rates were lower in the IJV group.
Conclusions: In light of the findings of the study implantable port placement via internal jugular vein is safe and had lower complication rates than either the subclavian or external jugular veins.
Introduction
According to Turkish statistics 167.463 new patients had cancer in 2015 [1]. Most of these patients are diagnosed in the late stages of their diseases. Therefore, chemotherapy comes about as the only treatment method for these patients. Because chemotherapy is a long-term treatment method the access site to administer the chemotherapeutics is important for patient comfort. The implantable venous sites are not only used to deliver chemotherapy regimens but also used to administer fluids, blood products and parenteral nutrition solutions.At the beginning subclavian vein was used fort port placement. But later on jugular vein gained popularity due to its advantages over subclavian vein. The aim of the study is to compare the duration and the complications of the implantable ports of subclavian and jugular veins.
Methods
After approval by the Ethics Committee (Institutional Review Board of Istanbul Education and Research Hospital of Health Sciences University26/10/2018-1481), we designed a retrospective cohort study and included 327 patients who had subcutaneous implantable ports (Power Loc® port access needle, C.R. BARD, Salt Lake City, Utah, USA) between April 2012 and April 2018. The ports were placed one of the three sites, subclavian, internal, or external jugular veins. The choice of the site was based on the initial surgery site, radiotherapy status, and the experience of the surgeon. All ports were placed by the same thoracic surgeon. Informed consent was taken from all patients. The files of the patients were evaluated retrospectively and age, gender, source of the primary tumor, access site, mean of catheter days, and complications were recorded.Most of the patients were referred by the oncologists. The thorough physical examinations of all patients were performed, and detailed medical and surgical histories were recorded. Complete blood count, routine blood chemistry, prothrombin time (PT), activated partial thromboplastin time (aPTT), international normalized ratio (INR), electrocardiography, chest X-ray were taken. All patients were consulted with an anesthesiologist.
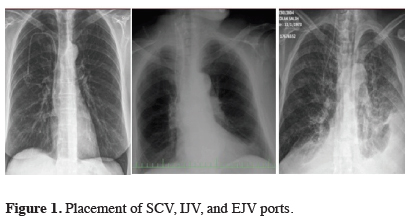
All procedures were in the operation room under sterile conditions. The patients were put in Trendelenburg position. The operation sites were cleansed with povidone-iodine twice and covered with sterile dresses. Local anesthesia was conducted with lidocaine hydrochloride 3mg/kg. Sedation was provided with midazolam 2-3 mg in un-cooperated patients. In all patients, venous entry was performed with an 18 G Seldinger needle and the tip of the guide-wire was advanced into the vena cava. After dilatation the catheter was placed into the vena cava. As for pocket preparation a 2-3 cm incision was made 5 cm below the clavicle. A tunnel was made between the venous site and the pocket by blunt and sharp dissection. The fatty tissue in the pocket was removed to place the port chamber. The catheter was connected to the port chamber with a trocar. The catheter was flushed with diluted heparin solution using a Huber needle. The Huber needle remained in the port chamber to prevent flip-over until the end of the procedure. The port chamber was fixed to the pectoral fascia by polyglactin sutures. The wound was closed with absorbable subcuticular sutures. Port efficacy was checked with an aspiration of blood, and the reservoir was flushed with heparin saline solution (9 cc 0.9% NaCl plus 1 cc heparin) to show any leakage. A chest x-ray was taken to check the position and the kinking of the catheter, and possibility of pneumothorax (Figure 1).
 Click Here to Zoom |
Figure 1: Placement of SCV, IJV, and EJV ports. |
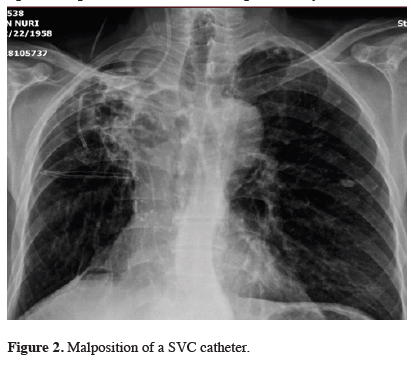
The malpositioned or kinked catheters were corrected under fluoroscopic guidance (Figure 2). The patient was discharged on the same day with paracetamol 500 mg, three times a day. Some catheters were placed during the operation performed to resect the pulmonary metastases.
 Click Here to Zoom |
Figure 2: Malposition of a SVC catheter. |
Statistical Analysis
Descriptive statistics were used, including mean ± standard deviation, median and range, frequencies and proportions. Chi-square test or Fisher’s exact test were used to compare the proportions and student t-test was used to compare the means. ANOVA was used to compare the groups. P < 0.05 is considered statistically significant.
Results
During the study period 327 patients had 342 implantation of ports either via subclavian vein (SC, 196 patients), internal jugular vein (IJC, 95 cases), and external jugular vein (EJV, 36 patients). The mean age of all patients was 55.86 ± 11.45 years. Male patients comprised 59% of the patients (193 cases). The 3 groups were homogenous in respect to age, sex, and intervention side (Table 1).Table 1: Clinical characteristics of the patients.
Colorectal cancers were the leading indications in all three groups, and gastrointestinal system followed them. Placing the port was faster in the ICV and EJV groups than the SC group, and the difference was significant. On the contrary, the port length was significantly longer in the ICV and ECV groups than SC group. Although occasion of port removal was least common in ICV group than the other 2 groups the difference did not reach significance.
Change of access site and the catheter malposition were leading complications in all patients (Table 2). Although catheter malposition was more common in the SC and EJV approach the difference was not found significant. Similarly the rate of pneumothorax was highest in the SC group. The chance of arterial injury was higher in the SC and EJV than the IJV group. An interesting complication called pinch-off (spontaneous fracture of an implanted central venous catheter) occurred in only one case of SC group and treated successfully with thoracotomy (Figure 3).
Table 2: Complications in 3 groups.
 Click Here to Zoom |
Figure 3: Removal of fractured catheter (pinch-off). |
Discussion
The management of the patient with cancer is challenging for physicians in terms of venous access that is not only for chemotherapy but also for administering blood products, antibiotics, fluids, and access to the bloodstream for clinical monitoring. The use of implanted ports provides comfort to the patients by preventing repeated venipunctures. During the last 2 or 3 decades the type and the structure of catheters have changed, the calibers and lumen numbers of the catheters have increased. The placement and care of the implantable ports requires a multidisciplinary approach including surgeons, nurses, oncologists, and anesthesiologists.According to the experience of the surgeon and the condition of the patient deep or superficial veins are used for entry sites. In the current study we started with the subclavian vein first and added the internal jugular vein, and used external vein in 36 patients in recent years. Our experience showed us that the best results were obtained by the IJV approach with the least complication rates. Li et al, in a 344-patient series, used SCV, IJV, and upper arm vein for access. They claimed that upper arm vein had superior to both IJV and SCV approach in terms of higher success rates and lower complication rates [2]. This study was a retrospective study like many other series in the literature.
A rare randomized study was reported from Biffi et al [3]. The study included 401 patients with 3 venous accesses; SCV, IJV, and cephalic vein. Unlike the findings of Li’s the Biffi reported that all 3 groups were similar with respect to success rates and complication rates. A similar study by Aribas et al. compared the IJV and SCV for patency times and complication rates and they pointed out that there was no difference between the 2 methods [4]. Another study comparing 145 patients with IJV to 165 EJV patients, and reported that the venous insertion site did not influence the early or late complication rates [5].
There are also series reporting the outcomes of single venous sites. One of the largest series in the literature was reported by Ahn and et al [6]. They placed 1254 venous ports under the guidance of ultrasound and fluoroscopy. They pointed out that the IJV approach is a safe and effective method with an extremely high technical success rate, low peri- and post-procedural complication rates, and satisfactory clinical outcome. Only 4% of the cases experienced early or late complications. In a similar study, Cil et al reported one of the highest success rate (99.8%) and lowest complication rate (0.63%) in the literature. The study was performed by radiologists and under ultrasound guidance [7]. IJV access could be either high or lower, and when appropriate high jugular approach was reported to be good alternative to low jugular approach [8]. Similar success rates were reported from another radiology department [9].
Keum et al reported a series with 242 patients who had 245 ports inserted via subclavian vein [10]. All ports were placed by a thoracic surgeon and no radiologic guidance was used. They reported 4.5% complication rate and recommended that the use of radiologic guidance could decrease the complications.
There some series and case reports in the literature reporting the use of superficial veins (external jugular and anterior jugular veins). Pancholi et al reported the use of external jugular vein in 23 patients and recommended its use with excellent safety and short procedure time [11]. Rott and Boecker reported a case and reviewed the literature about the use of anterior jugular vein [12].
An interesting complication of spontaneous fracture of an implanted central venous catheter (pinch off syndrome) occurred in one our patients with SCV group. The fractured part was in the Azygos vein and the attempt to remove by angiography was unsuccessful. We performed thoracotomy and removed the fractured catheter. This complication was reported in the literature [2,13]. Biffi also reported the cost-effectiveness of different access sites, and pointed out that subclavian vein approach was the most cost-effective method of central venous port placement and use [14].
American Society of Clinical Oncology (ASCO) published a clinical practice guideline for the central venous catheter care of the patient with cancer [15]. They pointed out there was insufficient evidence to recommend a specific type of CVC or insertion site, but femoral vein insertion should be avoided, except in certain emergency situations. They also recommended that port placement should be performed by well-trained health care providers, and not to give prophylactic use of systemic antibiotics before port placement.
This is a retrospective and non-randomized study. It comprised the cases during the learning curve. In the light of our findings port placement via the internal jugular vein is safe and the complication rate is lower than subclavian vein and external jugular vein. Though it was not found significant both malposition and pneumothorax rates are higher in the SCV and EJV groups.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) hsgm.saglik.gov.tr/depo/birimler/kanser-db/istatistik/Turkiye_Kanser_Istatistikleri_2015.pdf
2) Li Y, Cai Y, Gan X, Ye X, Ling J, Kang L et al. Application and comparison of different implanted ports in malignant tumor patients. World J Surg Oncol 2016; 14: 251.
3) Biffi R, Orsi F, Pozzi S,Pace U,Bonomo G, Monfardini L et al. Best choice of central venous insertion site for the prevention of catheter-related complications in adult patients who need cancer therapy: a randomized trial. Ann Oncol 2009; 20: 935-40.
4) Aribas BA, Arda K, Aribas O, Ciledağ N, Yoloğlu Z, Aktas E et al. Comparison of subcutaneous central venous port via jugular and subclavian access in 347 patients at a single center. Exp Ther Med 2012; 4: 675-80.
5) Karamustafaoglu YA, Yagci S, Kocal S, Yoruk Y. Comparison of implantable central venous ports: Subclavian versus Juguler access. J Clin Anal Med 2013; 4: 495-8.
6) Ahn SJ, Kim HC, Chung JW, An SB, Yin YH, Jae HJ et al Ultrasound and Fluoroscopy-Guided Placement of Central Venous Ports via Internal Jugular Vein: Retrospective Analysis of 1254 Port Implantations at a Single Center. Korean J Radiol 2012; 13: 314-23.
7) Cil BE, Canyigit M, Peynircioglu B, Hazirolan T, Carkaci S, Cekirge S et al. Subcutaneous venous port implantation in adult patients: a single center experience. Diagn Interv Radiol 2006; 12: 93-8.
8) Park HS, Kim Y, Lee Y, Kim JI, Seo H, Lee SM et al. Central venous infusion port inserted via high versus low jugular venous approaches: Retrospective comparison of outcome and complications. Eur J Radiol 2009; 72: 494–8.
9) Karaman B, Andic C, Oren NC, Battal B, Ustunsoz B. Subcutaneous infusion ports via the Internal Jugular Vein: Single center experience. EAJM 2010; 42: 78-80.
10) Keum DY, Kim JB, Chae MC. Safety of a totally ımplantable central venous port system with percutaneous subclavian vein access. Korean J Thorac Cardiovasc Surg 2013; 46: 202-7.
11) Pancholi M, Desai SM, Agrawal D, Mehta D, Pancholi A. External jugular venous cut down technique for placement of chemotherapy port and Hickman catheter: a study of 23 cases. World J Surg Oncol 2004; 2: 7.
12) Rott G, Boecker F. Port placement via the anterior jugular venous system: case report, anatomic considerations, and literature review. Case Rep Radiol 2017; 2017: 2790290.
13) Besirli K, Demirkaya A, Demirbas MY, Kilic Z. Pinch-off syndrome: an unusual complication following central venous port implantation. Türk Gogus Kalp Dama 2010; 18: 229-31.



