Summary
Gunshot injuries are the second most common cause of death following motor vehicle accidents. Embolization due to gunshot bullet is rarely reported in the literature. A 20-year-old male patient admitted to hospital due to chest pain where radiologic examinations demonstrated a bullet in his thorax. We learned that he was shot from his leg in Syrian civil war one year ago. This very interesting case of bullet embolism with its migration to left ventricle was reported.Introduction
War is a shame of humanity. 190 million people have died in 21th century due to wars and most of them were civilians. Injuries depended on gunshot are the second most common cause of death following motor vehicle accidents. Bullet embolism which is a rare but serious complication of penetrating trauma [1]. Most of the bullet embolisms are arterial and the victim has symptoms of ischemia. Venous bullet embolization is rare and generally the patient has no symptoms. However, if the bullet in the venous system migrates to the pulmonary artery it might cause serious problems [2].Herein, we present a 20-year old male patient presented with chest pain where the radiologic examinations demonstrated a bullet in his thoracic cavity. We learned that, he was shot from his leg one year ago. He has no other injuries, i.e. gunshot, in his entire body. We discussed this very interesting case within the light of relevant literature.
Case Presentation
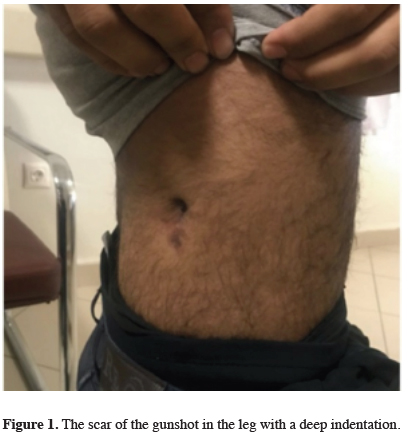
A 20-year-old male with a history of gunshot injury of leg one year ago in Syrian civil war, admitted to the clinic with the complaint of mild chest pain. He didn’t receive any medical treatment after this injury. The physical examination was normal except the scar of the wound in his right upper leg with a deep indentation which resembles a direct entrance (Figure 1). There was no scars to be accepted as an exit.
 Click Here to Zoom |
Figure 1: The scar of the gunshot in the leg with a deep indentation. |
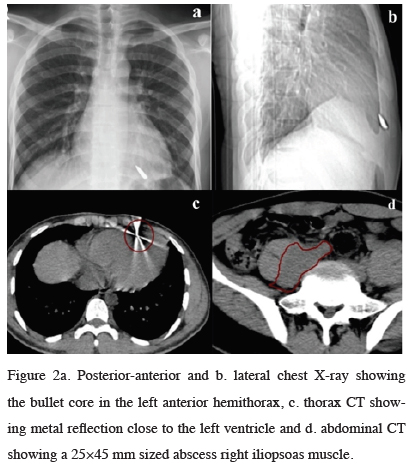
The posterior-anterior (Figure 2a) and lateral (Figure 2b) chest X-ray examinations demonstrated a bullet core in the left anterior hemithorax. The thorax computed tomography (CT) (Figure 2c), showed a metal reflection close to the left ventricle and abdominal CT showed a 25×45 mm sized abscess formation in his right iliopsoas muscle (Figure 2d).
 Click Here to Zoom |
Figure 2a: Posterior-anterior and b. lateral chest X-ray showing the bullet core in the left anterior hemithorax, c. thorax CT showing metal reflection close to the left ventricle and d. abdominal CT showing a 25×45 mm sized abscess right iliopsoas muscle. |
The echocardiography was normal and the bullet was seen not in his hearth chambers. Antibiotic treatment for the iliopsoas abscess was initiated.
An anterior approach via mediastinotomy was performed. During the peroperative exploration the bullet was seen within the myocardium of the left ventricular floor and consulted to cardiovascular surgery department. Eventually we left the bullet due to the close proximity to the left anterior descending artery. The first year follow up was uneventful.
Discussion
Thomas Davis reported a wood fragment embolism to the right ventricle in 1834 for the first time [1]. Many foreign bodies such as needles, intravenous catheters, bone fragments and bullets that migrate to the right ventricle were reported [3].A review has reported 0.3% incidence of foreign body migration during Vietnam war [1,4]. Bullet migration usually occurs immediately after trauma, but late migrations up to 14 years have been reported [1]. Bullet embolus can enter to the venous system nearly from any point of the injury by direct protrusion or by erosion of the vascular wall [5]. Various embolus pathways had been described in literature. These pathways are; from a peripheral vein to the heart [3,6], from a peripheral veins to the pulmonary artery [2], from a peripheral vein to another peripheral vein [7], paradoxical embolization from the right side to the left side [1] and from the heart to a peripheral veins [8].
Bullet core embolization must be suspected in gunshots entrance wounds without an exit or the final location of bullet does not confirm the expected pathway. Symptoms are associated with the location of the embolus. Arterial embolizations commonly presented with ischemic symptoms and venous embolism presented with valvular destruction, endocarditis, sepsis, venous thrombosis, dysrhythmia [3].
Management of foreign bodies in cardiovascular system depends on location and size of the foreign body. Common decision is to remove the foreign body. Knottnerus and colleagues suggest that follow up of the clinical course during an appropriate period is a good alternative. But some authors suggest that follow up of the clinical course is an alternative if the patient is symptomless [9]. There are such series of follow up to 20 years after Second World War where pericarditis was reported with an incidence of 25% [10]. Similar follow up series were also reported where no complications encountered [11]. Endovascular treatment is another option for the embolization of pulmonary artery and cardiac chambers [4,12]. The mortality of bullet embolism is 6% and mortality rate decreases 1-2% if the bullet is removed [13].
In conclusion bullet cores should be removed if they are symptomatic by considering profit and loss statement. If there is a risk of infection, embolization, or erosion even asymptomatic bullet cores should be removed. However, asymptomatic, risk free or late diagnosed cases might be treated conservatively.
Declaration of conflicting interests
The authors declared no conflicts of interest with re¬spect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Appendix. Conference Discussion
Dr. Özpolat (Editor-in-chief, Kırıkkale, Turkey): Dr. Balta, this is an interesting case report presenting the migration of a bullet to the heart. Could you give the details of intra operative findings?
Dr. Balta: I performed a mediastinotomy from the fourth intercostal space. After opening the pericardium at the left ventricle apex, I palpated the bullet. The cardiovascular surgeons were invited to the operating theatre. Unfortunately due to the localization of the bullet they suggested that it could cause a catastrophe if it was removed on beating heart.
Dr. Özpolat: Dr. Şimşek, could you make a suggestion about the migration of the bullet to the left heart via the venous circulation?
Dr. Şimşek (Kırıkkale, Turkey): This is a case of paradoxical embolus and the most possible pathway for the bullet to pass to arterial circulation is via a patent foramen ovale.
Dr. Özpolat: Dr. Şimşek, why does an echocardiography miss a foreign object?
Dr. Şimşek: Transthoracic echocardiography, being not only a subjective diagnostic tool but also having a weak power in imaging apical views, can lead to missing a foreign object especially in the left ventricular apex.
Dr. Özpolat: Dr. Doğan, during the preoperative work up what other studies could be performed?
Dr. Doğan (Ankara, Turkey): First, a venography of the lower extremity shows the structure of the vein, helps to detect any possible venous anomaly and venous thrombosis. Second, a preoperative transesophageal echocardiography (even perioperative) shows a possible septal defect for migration of the bullet core to left side of the heart.
Dr. Özpolat: Dr. Şahan, could we use cardiac MR, to evaluate the exact localization of the foreign object within the heart and to decide a plan for the surgical intervention?
Dr. Şahan (Kırıkkale, Turkey): The majority of bullets tested were found to be contaminated by ferromagnetic metals and some contain steel. If such a metallic object is located near or within a vital anatomic structure, it has the potentially to move. Caution is advised as well as an assessment of risk versus beneft for the patient is mandatory. Every case should be interpreted on its basis and if we have no idea about the content of the bullet, I will defnitely refuse to perform an MR.
Dr. Özpolat: Dr. Doğan, is it possible to remove a bullet from this localization on beating heart?
Dr. Doğan: It is exactly impossible to remove such an object when heart is beating. In such a situation, I just increase the length of the incision, place a pulmonary artery plus a femoral artery catheter for venous and arterial cannulations, give the cardioplegia solution and clamp the ascending aorta then via a small incision remove the foreign object from the apex of the left ventricle.
Dr. Özpolat: Dr. Şimşek, depending on the author’s conclusion which states “asymptomatic, risk free or late diagnosed cases might be treated conservatively”, should we give any other treatment to the patient?
Dr. Şimşek: I think, if the bullet was totally embedded in the myocardium no additional treatment is necessary. However, if a fragment is in the ventricle which should be confrmed via transesophageal echocardiography, warfarin should be prescribed just like the common follow up of mechanical prosthetic heart valves, in order to
prevent thrombus formation.
Affiliations;
Rıza Doğan, MD, Professor of Cardiothoracic Surgery, Hacettepe University Faculty of Medicine, Ankara, Turkey
Berkant Özpolat, MD, Professor of Thoracic Surgery, Kırıkkale University Faculty of Medicine, Kırıkkale, Turkey
Mehmet Şahan, MD, Assistant Professor of Radiology, Kırıkkale University Faculty of Medicine, Kırıkkale, Turkey
Vedat Şimşek, MD, Associate Professor of Cardiology, Kırıkkale University Faculty of Medicine, Kırıkkale, Turkey
Reference
1) Mattox KL, Beall AC Jr, Ennix CL, DeBakey ME. Intravascular migratory bullets. Am J Surg 1979; 137: 192-5.
2) Agarwal SK, Singh A, Kathuria M, Ghosh PK. Wandering bullet embolizing to the pulmonary artery: a case report. Asian Cardiovasc Thorac Ann 2007; 15: 154-6.
3) Howanitz EP, Murray KD, Galbraith TA, Myerowitz PD. Peripheral venous bullet embolization to the heart: case report and review of the literature. J Vasc Surg 1988; 8: 55-8.
4) Fernandez-Ranvier GG, Mehta P, Zaid U, Singh K, Barry M, Mahmoud A. Pulmonary artery bullet embolism-Case report and review. Int J Surg Case Rep 2013; 4: 521-3.
5) Miller KR, Benns MV, Sciarretta JD, Harbrecht BG, Ross CB, Franklin GA, et al. The evolving management of venous bullet emboli: a case series and literature review. Injury 2011; 42: 441-6.
6) Padula RT, Sandler SC, Camishion RC. Delayed bullet embolization to the heart following abdominal gunshot wound. Ann Surg 1969; 169: 599-602.
7) Harken DE. Foreign bodies in, and in relation to, the thoracic blood vessels and heart. Surg Gynecol Obstet 1946; 83: 117-25.
8) Chivukula S, Kaplan,S. Arterial bullet embolus following gunshot injury to the heart. Contemp Surg 1986; 29: 85-8.
9) Lundy JB, Johnson EK, Seery JM, Pham T, Frizzi JD, Chasen AB. Conservative management of retained cardiac missiles: case report and literature review. J Surg Educ 2009; 66: 228-35.
10) Bland EF, Beebe GW. Missiles in the heart: a twenty-year follow-up report of World War II cases. N Engl J Med 1966; 274: 1039-46.
11) Kortbeek JB, Clark JA, Carraway RC. Conservative management of a pulmonary artery bullet embolism: case report and review of the literature. J Trauma 1992; 33: 906-8.






