2Department of Pathology, Kırıkkale University Faculty of Medicine, Kırıkkale, Turkey DOI : 10.26663/cts.2019.00029
Summary
Amyloidosis is a disease characterized by extracellular accumulation of protein in fibrillary structure (amyloid protein) in various organs and soft tissues. Although the involvement of respiratory system is encountered in systemic amyloidosis, localized pulmonary amyloidosis has rarely been reported. The radiologic findings are nonspecific and show variations according to involvement pattern of amyloidosis. Here we present a 62-year-old female diagnosed as pulmonary nodular amyloidosis with the help of relevant literature.Introduction
Amyloidosis is a systemic disease characterized by extracellular deposition of abnormal protein fibrils -termed as amyloid protein- in various organs and tissues. Amyloid aggregates are insoluble and resistant to proteolysis. Although systemic amyloidosis is common and respiratory system is one of the affected tissues, certain forms are exclusively localized. Localized pulmonary nodular amyloidosis can be multiple or solitary. Peripheral or subpleural involvement is more frequent in lower lobes, which grow slowly. However, systemic type shows a diffuse alveolar septal involvement and radiologic changes may be absent [1-4].Here we present a case of pulmonary nodular amyloidosis and discussion of the radiologic, invasive diagnostic and pathologic features of this rare disease with the help of relevant literature.
Results
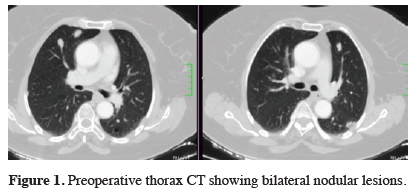
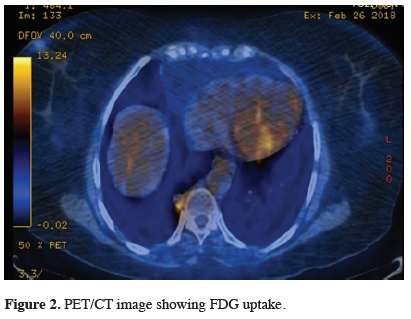
A 62 year-old female with non-productive cough with a 6-month history was referred to our clinic with thoracic CT findings of nodular opacities. The physical examination was normal other than bilaterally heard rhonchi. The biochemical values were normal. The thoracic computed tomography showed bilateral pulmonary nodules of different sizes with irregular contours and some having microcalcifications. The largest nodule was 24x22 mm (Figure 1). Abdominal CT was normal. PET/CT reported that the lesion at right mediobasal segment showed increased FDG avidity with SUV max of 4.0 (Figure 2).
 Click Here to Zoom |
Figure 1: Preoperative thorax CT showing bilateral nodular lesions. |
 Click Here to Zoom |
Figure 2: PET/CT image showing FDG uptake. |
Fiberoptic bronchoscopy revealed non-diagnostic bronchoalveolar lavage for malignancy and minimal chronic inflammation was reported.
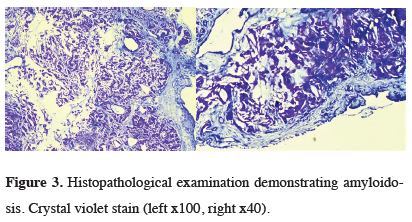
VATS wedge resection of two lesions one being the larges nodule with FDG uptake was performed which both were consisted with amyloidosis. Histologically the lesions were irregular nodules with diffuse acellular material accumulation at stroma and at wall of the vessels and, the lesions had limitations by mesothelial cells. On crystal violet stain, this deposit was confirmed to be amyloid. The final histopathologic diagnosis was pulmonary amyloidosis (Figures 3a,b). After the operation, the patient was referred to internal medicine department and the workup did not identify systemic amyloidosis. The 9th month follow up was uneventful with stabile nodules on control thoracic CT (Figure 4).
 Click Here to Zoom |
Figure 3: Histopathological examination demonstrating amyloidosis. Crystal violet stain (left x100, right x40). |
 Click Here to Zoom |
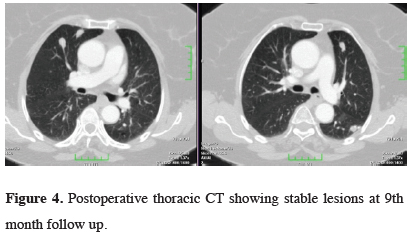
Figure 4: Postoperative thoracic CT showing stable lesions at 9th month follow up. |
Discussion
Amyloidosis is a disease characterized by extracellular deposition of amyloid protein in tissue and organs such as kidney, liver, spleen, lung, gastrointestinal tract, endocrine organs, skin, heart or the autonomous nervous system [1,2]. Many types of amyloid have been described and all share the characteristics of fibrillary B-pleated sheet configuration. Although the involvement of respiratory system is encountered in systemic amyloidosis, localized forms such as pulmonary amyloidosis has rarely been reported. Four histopathologic forms of respiratory amyloidosis defined as; a. focal deposits in tracheobronchial tree, b. diffuse parenchymal deposits, c. single or multiple parenchymal nodules and d. senile form [2]. Amyloid generally found in alveolar interstitium at the periphery of the nodule. As compact amyloid mass consists of many giant cells, lymphocytes and plasma cells normal parenchymal structure generally does not exist at the central parts [3]. Congo red and crystal violet stains are used to demonstrate amyloid [5]. As the present case is a multinodular form, we will concentrate on this form in this report.In nodular form the clinical signs and symptoms are nonspecific compared to other forms and although the patients are generally asymptomatic, cough, dyspnea and hemoptysis are the main complaints [2,6]. In this case, cough is the main symptom for a duration of 6 months.
The diagnosis of localized respiratory form is particularly difficult unlike the systemic form where in the systemic form workup involving blood, urine and imaging studies are generally diagnostic [3].
In the differential diagnosis of the multiple nodules showing calcifications, granulomatous diseases, tuberculosis, histoplasmosis, coccidiodomycosis, blastomycosis must be kept in mind. Multifocal calcifications are extraordinary in metastatic disease other than osteogenic sarcoma and chondrosarcoma. Lymphoproliferative diseases frequently accompanies multinodular form of the disease. In such cases, amyloidosis may be seen with parenchymal bullae or thin walled air cysts however the mechanism is not clear but hypothesized as, first, the occurrence of check valve mechanism due to the narrowed airway as a result of accumulation of inflammatory cells, second, increased alveolar wall destruction due to deposition of amyloid at alveolar wall and third, ischemic alveolar destruction due to deposition of amyloid at muscular wall of small blood vessels [3]. In the workup of this case, we did not identify such a co-existence.
Among radiologic imaging techniques HRCT makes the distinction of 5 types of nodular form; a. peripheral and subpleural localization which is generally bilateral and at the lower lobes, b. well defined, lobulated form, c. nodular form showing central (generally) or irregular calcifications, d. multiple nodules between 0.5 to 15 cm and e. slow growing nodular form without regression. Although mediastinal LAP is seen in 20% of amyloidosis, in localized form this is unusual and the presence should direct the surgeon to investigate the etiology [3,4].
Although calcifications in the nodules and other imaging and blood test did not support a primary malignancy, PET/CT was included to the diagnostic work up and the lesion at right mediobasal segment showed increased FDG avidity with SUV max of 4.0. Positive FDG uptake of pulmonary amyloidosis mimicking lung metastasis was rarely reported in the literature [4].
In amyloidosis fine needle aspiration biopsy has low field in diagnosis. Although CT-guided biopsies are reported to have a better chance of providing diagnostic material, most cases of pulmonary amyloidosis have been diagnosed only following surgical resection or at autopsy [1,2,4,7,8]. Similarly, in our case the final diagnosis was achieved following surgical resection. The nodule with positive uptake with high suspicion of malignancy and another one in the same lobe both were resected via VATS.
In systemic amyloidosis with respiratory involvement mean life expectancy was 16 months, however, in local form it is better. Mortality is due to obstruction of the airways and respiratory insufficiency [3,9]. To date there is still no effective treatment for systemic cases. Colchicine, melphalane and systemic steroid therapy and, conservative surgical excisions to protect the functional structure may be an option [5,9,10]. In this case, at the 9th month, follow up the nodules had remained stable at CT and annual radiologic controls was planned.
In conclusion, localized nodular pulmonary amyloidosis may mimic many benign and malign pulmonary disease radiologically without having clinical symptoms. In the differential diagnosis of multiple pulmonary nodules, localized amyloidosis should be kept in mind. Surgery plays an important role in the diagnosis.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Endicott KM, Hynes CF, Hsieh CM, Paal E, Trachiotis G. Two cases of monoclonal nodular pulmonary amyloidosis and review of the literature. Chest Disease Reports 2016; 4: 5945.
2) Bhavsar T, Huang Y, Gaughan C, Inniss S, Thomas R. Bilateral pulmonary nodular amyloidosis: A case report and review of the literature. World J Respirol 2012; 2: 6-8.
3) de Almeida RR, Zanetti G, Pereira E Silva JL, Neto CA, Gomes AC, Meirelles GS, et al. Respiratory Tract Amyloidosis. State-of-the-Art Review with a Focus on Pulmonary Involvement. Lung 2015; 193: 875-83.
4) Seo JH , Lee SW, Ahn BC, Lee J. Pulmonary amyloidosis mimicking multiple metastatic lesions on F-18 FDG PET/CT. Lung Cancer 2010; 67: 376-9.
5) Demirtaş S, Kutlu O, Sakin A. Trakeobronşial amiloidoz. İstanbul Med J 2015; 16: 119-21.
6) Kadiroğlu AK, Yıldırım Y, Yılmaz Z, Kayabaşı H, Avcı Y, Yıldırım MS, Yılmaz ME. A rare cause of secondary amyloidosis: common variable immunodeficiency disease. Case Rep Nephrol 2012; 2012: 4. doi: 10.1155/2012/860208.860208.
7) Guidelines Working Group of UK Myeloma Forum; British Commitee for Standards in Haematology, British Society for Haematology. Guidelines on the diagnosis and management of AL amyloidosis. Br J Haematol 2004; 125: 681-700.
8) Hajjar WM, Al-Johani TE, Jameel MA, Almutairi OT, Ahmed I, Hajjar AW, Al-Nassar SA. Pulmonary Nodular Amyloidosis Mimicking Metastatic Lung Lesion in a Patient with Colon Cancer. J Coll Physicians Surg Pak 2018; 28: 322-4.






