Summary
Neoplastic and non-neoplastic pathologies can cause lesions in the mediastinum. Bronchogenic cysts, germ cell tumors, lymphoma, lymph node hyperplasia, thymoma, thymic cysts, and thyroid masses tend to develop in mediastinal compartments. Tuberculosis would cause lymph node enlargement in many areas of the body but it is a very rare cause of mediastinal mass. We report a case of tuberculosis presenting with isolated, large middle mediastinal mass with high FDG uptake in PET/CT. We also present a short review of reported cases of mediastinal tuberculosis.Introduction
The mediastinum is the central compartment of the thoracic cavity that was divided into three compartments as anterior, middle and posterior. Different anatomical classifications of the mediastinum are reported in the literature [1]. These classifications are helpful in clinical practice to classify the mediastinal pathologies.The middle mediastinum is located in between pericardium in anterior and vertebral body in posterior. Bronchogenic cysts, bronchogenic tumors, lymph nodes, vascular masses and pleuropericardial cysts tend to develop in this mediastinal compartment. Tuberculosis would cause lymph node enlargement in different parts of the body, but it is very rare cause of mass in the middle mediastinum [2]. We report a case of tuberculosis that presenting with isolated, large middle mediastinal mass with high FDG uptake in PET/CT.
Case Presentation
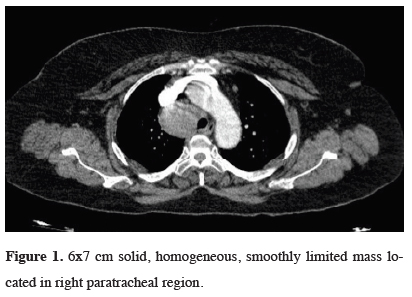
A 67-year-old female presented with complaints of breathlessness and chest pain for the last four months was referred to our department. The patient was a non-smoker, and there was not any history of chronic illness, prior hospitalization or surgery. Her family history was also non-significant. The laboratory tests showed only leukocytosis (13.0 × 109/ L) and mild anemia (hemoglobin 11g/dL). Chest radiogram revealed mediastinal enlargement, so thorax computed tomography is taken. Thorax CT is revealed a 6x7 cm solid, homogeneous, smoothly limited mass located in the paratracheal region in the middle mediastinum (Figure 1).
 Click Here to Zoom |
Figure 1: 6x7 cm solid, homogeneous, smoothly limited mass located in right paratracheal region. |
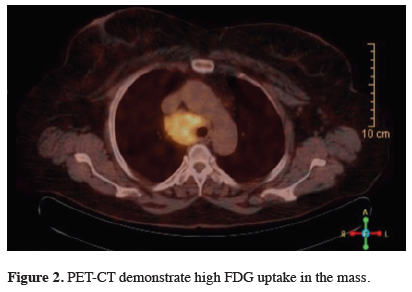
There were no invasion of structures such as the phrenic nerve, major vascular structures, lung, or sternum. To differentiate malign and benign conditions, PET-CT reported a high FDG uptake (Figure 2).
 Click Here to Zoom |
Figure 2: PET-CT demonstrate high FDG uptake in the mass. |
Because of the paratracheal localization of the mass, EBUS-TBNA is performed, but the diagnostic sample could not be obtained. So surgical excision was planned to make a definite diagnosis and alleviate symptoms of the mass effect.
Surgical Technique
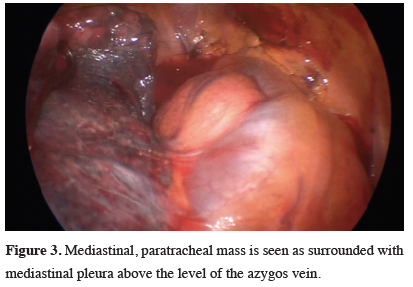
Video-assisted thoracoscopic surgery was performed with a selective intubation. The first incision, about 3-4 cm long was performed at the 4th intercostal space in the mid-axillary line to have a good access for the dissection of the middle mediastinum. The second incision was performed in the 7th intercostal space, in the mid-axillary line and was used as a camera port. The thoracic cavity was inspected visually and mediastinal, paratracheal mass was seen as surrounded by the mediastinal pleura above the level of the azygos vein (Figure 3).
 Click Here to Zoom |
Figure 3: Mediastinal, paratracheal mass is seen as surrounded with mediastinal pleura above the level of the azygos vein. |
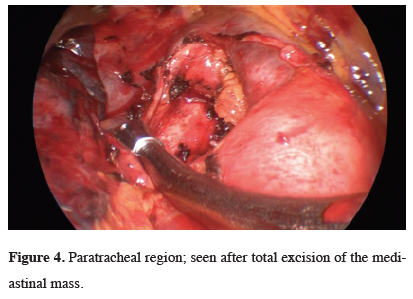
Mediastinal pleura was incised and the mass was freed up from superior vena cava and azygos vein with blunt and sharp dissection. The mediastinal mass was totally excised and the rapid diagnostic procedure performed via frozen section (Figure 4).
 Click Here to Zoom |
Figure 4: Paratracheal region; seen after total excision of the mediastinal mass. |
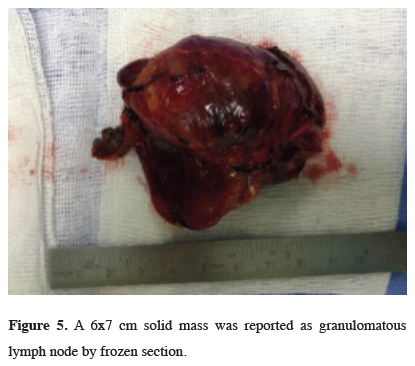
The frozen section reported that, the mass excised from middle mediastinum is a granulomatous lymph node secondary to tuberculosis infection (Figure 5).
 Click Here to Zoom |
Figure 5: A 6x7 cm solid mass was reported as granulomatous lymph node by frozen section. |
After the air leakage and hemorrhage control, a 28 French chest tube was inserted into the thoracic cavity through the camera port.
Postoperative Follow-up
The postoperative course was uneventful. The chest tube was removed on the post-operative day 2, and the patient was discharged on the postoperative third day.
Discussion
Neoplastic and non-neoplastic pathologies can cause lesions in the mediastinum. It is usually difficult to make a definitive diagnose due to the wide range of etiologies. Bronchogenic cysts, bronchogenic tumors, lymph nodes, vascular masses and pleuro-pericardial cysts may present as a large mass in the middle mediastinum [1]. In most of the cases patients don’t have any symptoms and mediastinal lesions are usually detected incidentally. If the lesion is large enough to make a compression to neighboring structures clinical presentations like chest pain, dyspnea and cough would be seen.Chest computed tomography (CT) is a valuable imaging modality for the evaluation of mediastinal masses. Also, magnetic resonance imaging (MRI) are used to distinguishing cystic from solid masses and to prove invasion to mediastinal structures especially in malign conditions.
Fluorodeoxyglucose (FDG) - positron emission tomography (PET) is helpful to make a differential diagnosis and evaluation of treatment response, especially in malign conditions like thymoma and germ cell tumors. Because of metabolic activity of inflammatory cells are increased FDG uptake also seen in a granulomatous disease like sarcoidosis and tuberculosis. Tuberculosis is the common cause of peripheral lymphadenopathy, especially in developing countries. However, tuberculosis presenting as a large mediastinal mass is a rare condition.
In literature 11 cases of isolated mediastinal mass were reported [3-13]. In four cases, mediastinal mass was excised with thoracotomy. In other cases only a punch biopsy was performed (Table 1).
To the best of our knowledge, this might be the first case of total excision of a mediastinal mass with VATS procedure and diagnosed as tuberculosis,. The important point for performing a VATS procedure is the advantage of decreased postoperative pain and a shorter hospital stay as known [14].
Total excision of a mediastinal tuberculosis is not necessary in all cases. However, if the patient has compression signs and the diagnostic sample could not be obtained with biopsy, surgical excision should be needed.
In conclusion, establishing the etiology of mediastinal masses can be difficult. Imaging techniques including CT, MRI, and PET-CT narrow the possible causes, but definitive diagnosis is performed only with histopathological verification. If total excision is planned, VATS is a safe and feasible procedure even for large masses as in our case. We aimed to present this case in the immunocompetent patient presenting with an isolated mediastinal mass. We also recommend the use of VATS when surgical excision is required.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Carter BW, Benveniste MF, Madan R, Godoy MC, de Groot PM, Truong MT, et al. ITMIG Classification of Mediastinal Compartments and Multidisciplinary Approach to Mediastinal Masses. Radiographics 2017; 37: 413-36.
2) Erbay M, Özsu S, Ayaydın Mürtezaoğlu ES, Türkyılmaz A, Özçelik N, Bülbül Y, Ersöz Ş. Causes of mediastinal/hilar granulomatous lymphadenitis. Tuberk Thoraks 2018; 66: 212-6.
3) Vincken W, Vandenbrande P, Roels P, Pirngadi J, Welch W. Isolated paratracheal mass of tuberculosis origin in an adult patient. Eur J Respir Dis 1983; 64: 630-5.
4) Thirithuvathas AJ, Ravikumar S, Gnanaseelan T. Huge prepericardial tuberculosis abscess in a 2-year-old child. J Pediatr Surg 1989; 24: 1124.
5) Ahmed A, Mirza S, Rothera MP. Mediastinal tuberculosis in a 10- month-old child. J Laryngol Otol 2001; 115:161-3.
6) De Ugarte DA, Shapiro NL, Williams HL. Tuberculous mediastinal mass presenting with stridor in a 3-month-old child. J Pediatr Surg 2003; 38: 624-5.
7) Maeder M, Ammann P, Rickli H, Schoch OD. Fever and night sweats in a 22-year-old man with a mediastinal mass involving the heart. Chest 2003; 124: 2006-9.
8) Gillies MJ, Farrugia MK, Lakhoo K. An unusual cause of a superior mediastinal mass in an infant. Pediatr Surg Int 2008; 24: 485-6.
9) Boussetta K, Tinsa F, Ghaffari H, Brini I, Aloui N, Jaubert F, et al. Mediastinal tuberculosis mass in a three-month-old boy. Tunis Med 2010; 88: 602-4.
10) Khilnani GC, Jain N, Hadda V, Arava SK. Anterior mediastinal mass: a rare presentation of tuberculosis. J Trop Med 2011; 2011: 635385.
11) Kumar N, Gera C, Philip N. Isolated mediastinal tuberculosis: a rare entity. J Assoc Physicians India 2013; 61: 202-3.
12) Jain N, Khilnani G, Hadda V, Iver V. Cystic mediastinal mass: a rare presentation of tuberculosis. Chest 2013; 144: 4.
13) Maguire S, Chotirmall SH, Parihar V, Cormican L, Ryan C, O’Keane C, et al. Isolated anterior mediastinal tuberculosis in an immunocompetent patient. BMC Pulmonary Medicine 2016; 16: 24.
14) Reddy RV. The advantages of VATS: a systematic review. Thorax 2005; 60: 238.






