

2Department of General Surgery, Ankara Numune Research and Training Hospital, Ankara, Turkey DOI : 10.26663/cts.2019.00016
Summary
We present a 57-year-old woman who has a giant mediastinal goiter, which lies down from cervical zone to right posterior mediastinum. On physical examination mediastinal goiter was nonpalpable. Giant mediastinal goiter was removed by right lateral thoracotomy, cervical collar incision and partial sternotomy. Pathology was reported as a multinodular goiter. We cannot perform VATS (video-assisted thoracoscopy) due to tight adhesion of the pleura. With the difference of literature partial sternotomy can be added to the transcervical and lateral thoracotomy approach for ease of removing giant posterior mediastinal goiters which lie down left cervical to the right posterior mediastinum.Introduction
Mediastinal goiters are grouped under two main headings which primary and secondary. Primary goiters root in an abnormal embryologic migration of the thyroid anlage. Secondary goiters develop from the descent of the thyroid into the mediastinum. Primary mediastinal goiter’s blood supply is from the mediastinal vessels in spite of this secondary mediastinal goiter’s blood supply from the cervical branch of arteria thyroidea. In the literature, the incidence of substernal goiter is reported between 0.2-45%. Primary mediastinal goiters are quite rare, occurring in less than 1% of all goiters. Secondary mediastinal goiters most commonly grow to anterior mediastinum, just 10-15% of these grow to posterior mediastinum [1].In this case report, we presented a quite rare giant posterior secondary mediastinal goiter, which lies down left cervical to the right posterior mediastinum and its surgical management.
Case Presentation
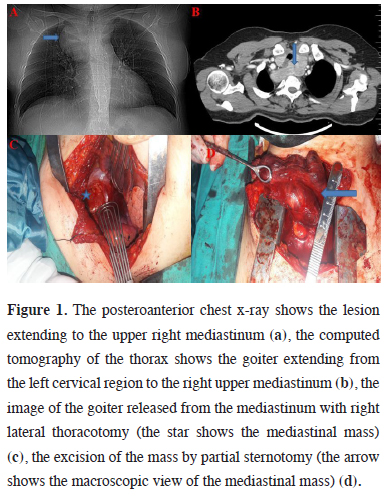
A 57-year-old woman presented with dyspnea and dysphagia. On physical examination, there wasn’t any palpable mass on her anterior neck. Thyroid ultrasonography showed that her both thyroid lobes had multiple, variable magnitude and hypoechoic /isoechoic solid nodules. The chest x-ray revealed a homogeneous opacity projecting on the right upper mediastinum. Computed tomography (CT) of the thorax demonstrated a large multinodular goiter, which enlisted in the upper mediastinum laminating the trachea and esophagus and displacing them to the anterior. It was in tight contact with the aortic arch and its left lower pole down into the posterior mediastinum and arrives below the carina (Figures 1a,b).
 Click Here to Zoom |
Figure 1: The posteroanterior chest x-ray shows the lesion extending to the upper right mediastinum (a), the computed tomography of the thorax shows the goiter extending from the left cervical region to the right upper mediastinum (b), the image of the goiter released from the mediastinum with right lateral thoracotomy (the star shows the mediastinal mass) (c), the excision of the mass by partial sternotomy (the arrow shows the macroscopic view of the mediastinal mass) (d). |
Ultrasonography-guided fine needle aspiration biopsy showed a multinodular colloid goiter. The patient consented for total thyroidectomy through a transcervical approach, and if necessary, transthoracic approach by both general and thoracic surgery teams. At first, a thyroidectomy was begun via a standard cervical approach. We could not perform VATS (video-assisted thoracoscopic surgery) due to tight adhesion of the pleura. Then we performed right lateral thoracotomy and partial sternotomy (Figures 1c,d).
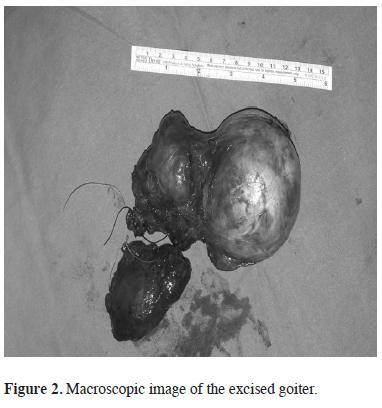
A lateral thoracotomy was performed to release the mass lesion from the thorax and a partial sternotomy incision was added to remove the mass from the neck incision. After excision of the goiter, we found that the right lobe was measured 6x4.5x3 cm, left lobe with mediastinal part was measured 13x10x4 cm (Figure 2).
 Click Here to Zoom |
Figure 2: Macroscopic image of the excised goiter. |
The patient was discharged at day 5. Histopathological examination reported a multinodular goiter. Fifteen months after surgery, the patient was asymptomatic and disease free.
Discussion
Most substernal goiters can be accessed via the collar incision but 2-29% requires additional incisions. These incisions can be lateral thoracotomy, partial or total sternotomy dependent on the placement of mediastinal goiters.Symptoms of secondary mediastinal goiters are dysphagia, dyspnea, and mass on the neck. Our patient did not have any mass on her neck but she had both dysphagia and dyspnea [2].
Computed tomography of the neck CT and are used for imaging. CT of the thorax provides information pointing toward the between anatomical structures and thyroid nature of the mediastinal mass [3]. Secondary mediastinal goiters lie down from cervical zone to the upper mediastinum and 50% of the lesion is under the aperture thoracica superior. These masses usually come by trachea and lie down to anterior mediastinum. Ten to fifteen percent of these extend to the right side of posterior mediastinum [4].
Negative thoracic pressure, gravity and the potential space in the thoracic cavity cause goiters to extend to the thoracic cavity. The posterior mediastinal extension is usually right-sided because of the presence of the aortic arch and pulmonary vessels on the left side obstructing the path of descent [5]. Machoda et al. reported that giant mediastinal goiters, which excised from left to right via the transcervical and lateral thoracotomy [4]. On the literature, there are some methods including VATS and RATS (robotic-assisted thoracoscopic surgery) [3].
In our case, the lesion was extremely big so that at first we started via VATS but we couldn’t perform VATS due to tight adhesion of the pleura because of this we added partial sternotomy to our operation approach for removing the mass easily.
This incision did not cause any complication but also made removing the giant flipped goiter easy.
In conclusion, we can add partial sternotomy to transcervical plus lateral thoracotomy approach to remove a giant multinodular goiter easily, which lies down from cervical zone to right posterior mediastinum.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Newman E, Shaha AR. Substernal goiter. J Surg Oncol 1995; 60:207-12.
2) Nakaya M, Ito A, Mori A, Oka M, Omura S, Kida W et al. Surgical treatment of substernal goiter: An analysis of 44 cases. Auris Nasus Larynx 2017; 44: 111-5.
3) Tsilimigras DI, Patrini D, Antonopoulou A, Velissaris D, Koletsis E, Lawrence D et al. Retrosternal goitre: the role of the thoracic surgeon. J Thorac Dis 2017; 9: 860-63.



