

Summary
A 45-year-old female patient is referred to our service for presenting seven months with left chest pain accompanied by dyspnea. At the chest tomography, a low-density mass with the presence of multiple vascularized septa, without evidence of tumor extension, without mediastinum nodes growth, neither metastatic lesions. The patient was operated with posterolateral thoracotomy. In the exploration, a 10x8x6 cm spherical mass was found which was solid, mobile, with pulmonary apical parenchyma peduncle, and it was totally excised. The postoperative pathology of the patient was reported as a pleuropulmonary solitary fibrous tumor. The management of this case took guidance from the Perrot’s recommendations, surgical resection is the mainstay treatment.Introduction
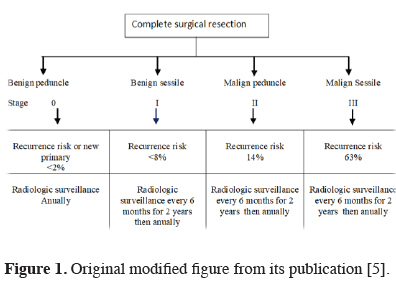
The pleuropulmonary solitary fibrous tumor is a mesenchymal origin tumor described by Klemperer and Rabin 1931 [1]. Approximately 900 cases have been documented in the literature up to 2005 [2]. It occurs between 50 to 60 years of age without gender predilection; it is not related to environmental, genetic, and occupational exposure. Its clinical presentation is pleuropulmonary symptomatology and its relationship to paraneoplastic syndromes; 20% pulmonary osteoarthropathy (Pierre-Mary-Bamberger Syndrome) and 5% refractory hypoglycemia (Doege-Potter Syndrome). 80% are benign. The diagnostic approach is with tomography or thoracic magnetic resonance and biopsy, with an immunohistochemistry panel, positive vimetine, CD34, BCL2 and negative keratin [3-9]. The histological dichotomy between benign and malignant should be avoided with the exception of the anaplastic tumor, which has aggressive behavior. Therefore, the malignancy of the solitary fibrous pleural tumor is defined as risk of aggressive or malignant behavior, and this is based on a set of clinical, histological and anatomical criteria, which are calculated with the following behavioral risk stratification models; England in 1989 (1 or more histological criteria), Perrot in 2002 (1 or more histological criteria) and Tapias in 2013 (3 or more of any histological or anatomical criteria). The histological criteria are; > 4 mitoses per 10 fields, Hypercellularity, necrosis, hemorrhage, vascular invasion and / or stroma. The anatomical criteria are; > 10 cm, sessile and parietal pleura [4]. Perrot classifies them as benign peduncle, benign sessile, malignant peduncle, and sessile malignant (Figure 1).
 Click Here to Zoom |
Figure 1: Original modified figure from its publication [5]. |
Tapias calculates the risk of recurrence with the presence of 3 or more criteria at 3, 5 and 10 years of 20%, 20% and 77% respectively, and 0% with the presence of less than three criteria [6].
Surgical resection is the cornerstone of the treatment, which can be curative if it is an R0 resection [4]. Metastases to liver, lung, and central nervous system are recognized [7]. So that, American Joint Committee on Cancer (AJCC)/ Union for International Cancer Control (UICC), recommends that the pleuropulmonary solitary tumor considered aggressive or malignant be approached with the TNM 8 for retroperitoneal sarcoma staging system [4]. In the case of incomplete surgical resections, postoperative radiotherapy can be offered [5]. However, multimodal or adjuvant therapy is controversial in a pleural solitary fibrous tumor. Therefore, each case must be individualized and treated in a multidisciplinary manner in the case of resection with incomplete margins or a recurrent tumor [4].
In this paper, we evaluated a very rare case of pleuropulmonary solitary tumor with literature.
Case Presentation
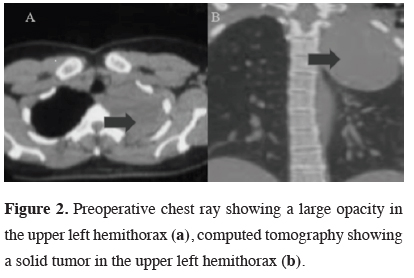
A 45-year-old female patient is referred to our service for presenting seven months with left sided chest pain accompanied by dyspnea on exertion. Chest X-ray evidences tumor located in the apical region of the left lung. The chest tomography reported a 9x8 cm low-density mass with the presence of multiple vascularized septa, without evidence of tumor extension, without mediastinum nodes growth, neither metastatic lesions (Figure 2).
 Click Here to Zoom |
Figure 2: Preoperative chest ray showing a large opacity in the upper left hemithorax (a), computed tomography showing a solid tumor in the upper left hemithorax (b). |
Transthoracic puncture lung biopsy reported mesenchymal cells compatible with a pleuropulmonary solitary fibrous tumor. Immunohistochemistry was vimentin positive and keratin negative. The patient was informed about the nature of the disease and its corresponding treatment and prognosis, so she accepts surgical resection. A preoperative protocol of pulmonary resection and thoracic surgery was performed. Functional and developmental status, Zubrod 1. Perioperative respiratory low-risk complications and no cardiovascular risk. Thoracoscore 0.1% and The National Surgery Quality Improvement Project (NSQIP) 4.5% risk for perioperative death.
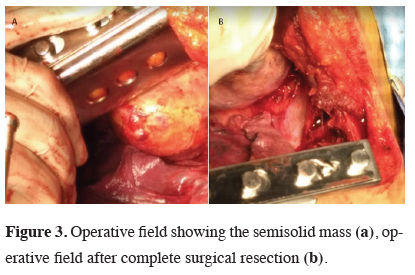
The patient was operated with posterolateral thoracotomy. In the exploration, a spherical mass was found, 10x8x6 cm, solid, mobile, with pulmonary apical parenchyma peduncle with lax adhesions to the mediastinum and anterior endothoracic fascia. Mediastinum without alterations (Figures 3,4).
 Click Here to Zoom |
Figure 3: Operative field showing the semisolid mass (a), operative field after complete surgical resection (b). |
 Click Here to Zoom |
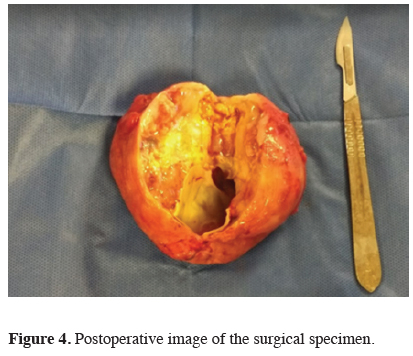
Figure 4: Postoperative image of the surgical specimen. |
Mass enucleation was possible without the need to resect lung tissue, structures of the mediastinum neither thoracic wall enblock resection. Hemostasis was verified, and leakage was ruled out, so that the thoracotomy was closed, leaving 32 FR pleural drainage. The patient had a 7-point surgical APGAR score with a 1% risk of complications and a 6% mortality rate. The patient was discharged postoperative 5 day without any complication. The histological report resulted in pleural macroscopic tumor origin, with 10x8x6 cm cystic dimensions with little serous material inside. Microscopically; visceral pleural cells origin with lipomatous characteristics, 2 mitoses per 10 fields, without areas of necrosis, neither stromal invasion. The risk of malignancy or aggressive behavior based on the Tapia model (<3 criteria) was 0%. The follow-up management was based on Perrot’s recommendations for benign pedunculated behavior with less than 2% risk of recurrence or new primary tumor, so the radiological control will be every six months for two years and later annually.
Discussion
Female case who presented chest pain and dyspnea as clinical manifestations. We decided to initiate the diagnostic protocol for lung cancer. This behavior was performed because in literature lung cancer has been occurring in people under 65 years of age without risk factors, and the prognosis of early treatment is favorable [8]. We defined pleural solitary fibrous tumor diagnosis, and proceed to a complete surgical resection as the Tapias recommendation [4,5]. We didn’t perform bronchoscopy due no tracheobronchial endoluminal alterations were detected at the tomography, neither tumor extension was detected in neighboring anatomical structures or growth of the short axis of the mediastinum lymph nodes.Surgical resection could be performed without difficulty. Post-surgical results had histological and anatomical criteria for benign mass. We opted for the Tapias model to stratify the risk of aggressiveness because it is the model recommended by the European Journal of Cardiothoracic Surgery, in which the risk of recurrence with less than three criteria, whether histological or anatomical is 0% with a P < .0001 [6]. Pleuropulmonary solitary fibrous tumor post-surgical follow-up is similar to lung cancer, which is radiological control every six months for two years and then annually. Post-treatment surveillance is recommended based on clinical and surgical criteria and TNM 8 recommendations [4]. In relation to adjuvant treatment, chemotherapy and radiotherapy have not been demonstrated as alternatives. However, it has been suggested that adjuvant radiotherapy may be an option in incomplete resections [5].
In conclusion, pleuropulmonary solitary fibrous tumor malignancy is based on the prediction of the aggressive behavior of the tumor based on a set of clinical, histological, and anatomical criteria. So that adequate knowledge of this pathological entity is crucial to grant an adequate diagnosis and treatment approach. Complete surgical resection is the cornerstone of the treatment. Multimodal therapy is controversial, and this is not recommended in an R0 resection of the pleural solitary fibrous tumor regardless of its risk stratification, the exception being incomplete resection, recurrence, and the anaplastic histological variant. In this case report, we found a patient with preoperative and postoperative diagnosis solitary fibrous tumor of the pleura benign peduncle. Which was managed with complete resection (R0) of the tumor by enucleation. Perioperative management of standard chest surgery without complications with post-surgical follow-up every six months with chest tomography with low radiation and then annually up to 5 years.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Klemperer P, Rabin CB. Primary Neoplasms of the pleura. A report of five cases. Am J Ind Med 1992; 22:4-31.
2) Sung SH, Chang J-W, Kim J, Lee KS, Han J, Park SI. Solitary Fibrous Tumors of the Pleura: Surgical Outcome and Clinical Course. Ann Thorac Surg 2005; 79: 303-7.
3) Samer K, Michael TJ. Pleural masses. In: Dolores M. editor. Medical management of the thoracic surgery patient. Saunders/Elseviere. Philadelphia PA; 2010. p. 435-437.
4) Tapias LF, Mercier O, Ghigna MR, Lahon B, Lee H, Mathisen DJ, et al. Validation of a scoring system to predict recurrence of resected solitary fibrous tumors of the pleura. Chest 2015; 147: 216.
5) Perrot MD, Fischer S, Bründler M-A, Sekine Y, Keshavjee S. Solitary fibrous tumors of the pleura. Ann Thorac Surg 2002; 74: 285-93.
6) Tapias LF, Mino-Kenudson M, Lee H, Wright C, Gaissert HA, Wain JC, et al. Risk factor analysis for the recurrence of resected solitary fibrous tumours of the pleura: a 33-year experience and proposal for a scoring system. Eur J Cardiothorac Surg 2012; 44: 111-7.
7) Lahon B, Mercier O, Fadel E, Ghigna MR, Petkova B, Mussot S, et al. Solitary Fibrous Tumor of the Pleura: Outcomes of 157 Complete Resections in a Single Center. Ann Thorac Surg 2012; 94: 394-400.



