2Department of Gastroenterology, Bozyaka Training and Research Hospital, Izmir Turkey
3Department of General Surgery, Bozyaka Training and Research Hospital, Izmir Turkey DOI : 10.26663/cts.2019.00129
Summary
Colonoscopy is a safe procedure and in less than 1% of the patients, colonic perforation may be seen. Physical examination findings such as pain and distension of the abdomen are well-known symptoms however, dyspnea and tachypnea are seen in only a small number of cases as a sign of iatrogenic colon perforation. In this report, we present a 70-year-old female patient with iatrogenic pneumoperitoneum, pneumomediastinum, subcutaneous emphysema and bilateral pneumothorax after diagnostic colonoscopy. The patient was successfully treated with endoscopic colon repair and left tube thoracostomy. When atypical findings are present such as dyspnea and subcutaneous emphysema, iatrogenic pneumothorax, pneumomediastinum should be kept mind after colonoscopy.Introduction
Colonoscopy is a standard diagnostic and therapeutic approach for gastrointestinal tract disorders and the number of colonoscopy use continues to grow rapidly. Colonoscopy is regarded a relatively safe procedure however, complications such as bleeding and perforation can occur. Perforation is one of the most serious complications and its incidence was shown as about <0.005% to 0.65% in the literature [1,3]. Perforation is especially associated with pneumoperitoneum, peritonitis and sepsis in most cases, requires surgical treatment and may be a lethal prognosis in advanced cases [2,3]. Pneumothorax, pneumomediastinum have been reported in few cases [4-6].In this report, we present a patient with bilateral pneumothorax, pneumomediastinum, subcutaneous emphysema, pneumoperitoneum due to iatrogenic colon perforation during diagnostic colonoscopy. Unfortunately, during the treatment of pneumothorax, an iatrogenic hemothorax also developed all iatrogenic injuries were treated successfully.
Case Presentation
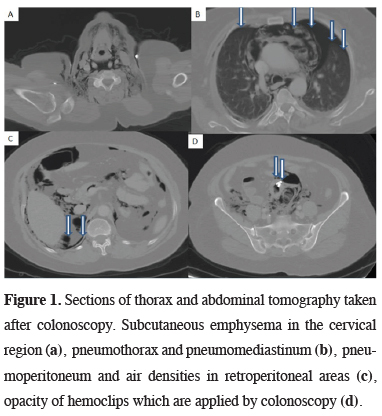
A 70-year-old female patient was admitted to the hospital with dyspeptic complaints and a moderate anemia (hemoglobin 10.4 g/dL, hematocrit 34.0%). Obesity, diabetes mellitus, suspected liver failure were obtained in her medical history. The patient underwent diagnostic colonoscopy with these findings and a diverticulum was detected in the sigmoid colon. During passing from diverticulum, a small perforation developed and this area was immediately repaired with hemoclips. After colonoscopic procedure, the patient was taken to the intensive care unit. Approximately 6 hours later, the patient described dyspnea. On physical examination, decreased respiratory sounds in the left hemithorax and subcutaneous emphysema on cervical area was obtained. Thorax computed tomography revealed subcutaneous emphysema in the cervical and infraclavicular region, mediastinal diffuse air densities, bilateral pneumothorax (left dominant) and bilateral minimal pleural effusion. Abdominal computed tomography showed diffuse pneumoperitoneum, minimal free intraabdominal fluid adjacent to the liver and density of metallic clips in the proximal part of the sigmoid colon (Figure 1).
 Click Here to Zoom |
Figure 1: Sections of thorax and abdominal tomography taken after colonoscopy. Subcutaneous emphysema in the cervical region (a), pneumothorax and pneumomediastinum (b), pneumoperitoneum and air densities in retroperitoneal areas (c), opacity of hemoclips which are applied by colonoscopy (d). |
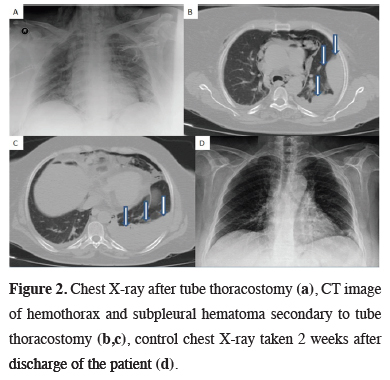
24F apical tube thoracostomy was performed under local anesthesia for treatment of left sided pneumothorax. The control chest X-ray showed complete expansion of the left lung (Figure 2). Antibiotic treatment was arranged and oxygen therapy was administered by for pneumomediastinum, pneumoperitoneum and subcutaneous emphysema. On the second postoperative day, pleural effusion and subpleural hematoma was seen on the chest radiography and a 32F thorax catheter was inserted to left hemithorax and approximately 500 cc of blood was drained (Figure 2). The patient was followed up on daily chest radiographs, hemogram and C- reactive protein levels.
 Click Here to Zoom |
Figure 2: Chest X-ray after tube thoracostomy (a), CT image of hemothorax and subpleural hematoma secondary to tube thoracostomy (b,c), control chest X-ray taken 2 weeks after discharge of the patient (d). |
The patient was followed by general surgeons and gastroenterologists on daily bases. Abdominal examination was normal and oral intake was allowed on the 4th day. Apical thorax catheter was terminated on the 3rd day and basal thorax catheter was terminated on the postoperative 5th day. The patient was discharged uneventfully. 6th month follow up of the patient as normal. A written consent form was obtained from the patient for this scientific publication.
Discussion
Colorectal perforation is one of the most serious complications of colonoscopy and usually presents with signs of peritoneal irritation [1-3]. Respiratory pathologies such as pneumothorax, pneumomediastinum and subcutaneous emphysema develop in only a minority of cases [2-6]. In the meta-analysis published by Ajay Gupta et al. [5] iatrogenic pneumothorax following colonoscopy were reported in only 21 cases.Colonoscopic perforation can occur by various mechanisms; direct mechanical trauma, thermal injury or barotrauma (because of massive air insufflation) [5,6]. Many factors such as old age, female sex, previous abdominal-pelvic surgery, adhesions, diverticulosis, severe colitis, inflammatory bowel disease, malignancy, radiation therapy, low albumin level etc. have been identified for increased risk [1-3,6,7]. Unfortunately, our patient had three risk factor together as; advanced age, colon diverticulum and female sex.
Perforations may be located in the intraperitoneal/extraperitoneal part of the colon, or occur with combination, although clinical signs and symptoms variable according to perforation location [1-3]. When perforation develop in the intraperitoneal part of colon, abdominal complaints may be the first symptoms such as pain, distension or rigidity but, if the perforation is in extraperitoneal part of the colon or rectum, atypical symptoms may develop such as dyspnea, tachypnea and subcutaneous emphysema [1,2,5].
The pathophysiological mechanism of subcutaneous emphysema and pneumomediastinum might be explained due to the presence of a visceral space, which goes from the neck through the mediastinum and retroperitoneum [4-8]. This visceral space follows the trachea and esophagus along the chest and creates a tract for air. The space continues inferiorly through the diaphragmatic hiatus and reaches to the retroperitoneum [4-8]. When air enters the retroperitoneum, it rises by pressure effect along the fascial planes, follows the large vessels, progress through the diaphragmatic hiatus, and reaches to the mediastinum and subcutaneous neck tissues [4-10]. Large amount of air may leak from the mediastinal pleura to the pleural cavity [5,8,9]. Alternatively, free air in the peritoneal cavity may permeate through to intrapleural cavity with small diaphragmatic defects or fenestrations. Air may spread to many places with similar mechanisms, and even cases with atypical findings such as pneumoscrotum have been reported [11].
Clinical suspicion, physical examination and radiologic findings are important in diagnosis. Accompanied by clinical findings, it has been reported that sub-diaphragmatic air in abdominal radiography is an important sign and can be diagnosed in approximately 87% of cases [2]. Chest radiography may also be helpful in cases who present with pneumothorax [3-7]. Abdominal computed tomography may provide information about the location of perforation [1-5].
Early diagnosis of colon perforation is an important issue and it also affects the choice of treatment likelihood; nonoperative management, primary repair, intestinal resection with a primary anastomosis or double stage procedure [2]. In only a rare portion of patients may diagnosed during the procedure like in our case. Corey W et al [2] examined 180 patients who developed colon perforation after colonoscopy and reported 140 of patients were diagnosed within 24 hours. Only 42 patients were diagnosed during colonoscopy. Peritonitis findings may progress and surgical treatment may become more difficult for general surgeons in patients with late diagnosis [2]. It has been reported most of the cases have to undergone surgical treatment and endoscopic repair can be performed in a very limited number of cases in the literature [1,2]. In this case, colonoscopy was performed by an experienced gastroenterologist, perforation was noticed during colonoscopy and repaired with endoscopic hemoclips. The patient was carefully followed up by the general surgery clinic after the procedure and there were no abdominal complaints.
For the treatment of pneumomediastinum and subcutaneous emphysema oxygen inhalation and supportive therapy were preferred in this patient. Since the etiology of pneumomediastinum was known and tracheobronchial injury was not suspected, additional diagnostic procedures such as bronchoscopy were not performed. For bilateral pneumothorax treatment, left tube thoracostomy was used and the patient was followed up with chest radiographs. Unfortunately, an iatrogenic hemothorax also developed in our patient secondary to tube thoracostomy. Therefore, a second tube thoracostomy was performed and the patient was treated without any additional problems.
In conclusion, follow-up period after colonoscopy is an important issue. Abnormal abdominal examination findings such as pain, distention, rebound, rigidity etc. are well known by gastroenterologists and general surgeons. Atypical findings such as subcutaneous emphysema, dyspnea, hoarseness, impaired voice quality may be seen in a small minority of patients. When these atypical findings are encountered, differential diagnosis such as pneumothorax, pneumomediastinum should be kept mind as a sign of iatrogenic colon injury. Cooperation with gastroenterologist, thoracic surgery and general surgery clinics will be effective in achieving successful results.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Hamdani U, Naeem R, Haider F, Bansal P, Komar M, Diehl DL, et al. Risk factors for colonoscopic perforation: a population-based study of 80118 cases. World J Gastroenterol 2013; 19: 3596-601.
2) Iqbal CW, Cullinane DC, Schiller HJ, Sawyer MD, Zietlow SP, Farley DR. Surgical Management and Outcomes of 165 Colonoscopic Perforations From a Single Institution. Arch Surg 2008; 143: 701-7.
3) Arora G, Mannalithara A, Singh G, Gerson LB, Triadafilopoulos G. Risk of perforation from a colonoscopy in adults: a large population-based study. Gastrointest Endosc 2009; 69: 654-64.
4) Choi PW. Pneumomedıastınum, pneumothorax, and subcutaneous emphysema caused by colonoscopıc perforatıon: a report of two cases. J Emerg Med 2017; 52: e117-e122.
5) Gupta A, Zaidi H, Habib K. Pneumothorax after Colonoscopy-A Review of Literature. Clin Endosc 2017; 50: 446-50.
6) Ho HC, Burchell S, Morris P, Yu M. Colon perforation, bilateral pneu¬mothoraces, pneumopericardium, pneumomediastinum, and subcu¬taneous emphysema complicating endoscopic polypectomy: anatomic and management considerations. Am Surg 1996; 62: 770-4.
7) Lee HS, Park HH, Kim JS, Kang SH, Moon HS, Sung JK, et al. Pneumoretroperitoneum, Pneumomediastinum, Pneumothorax, and Subcutaneous Emphysema after Diagnostic Colonoscopy Korean J Gastroenterol 2017; 70: 145-9.
8) Macklin, C. Transport of Air Along Sheaths of Pulmonic Blood Vessels from Alveoli to Mediastinum: Clinical Implication. Arch Intern Med 1939; 64: 913-26.
9) Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Intern Med 1984; 144: 1447-53.






