

Summary
Background: Cyst hydatid is an important health problem in childhood and adult age group. We aimed to present the management of childhood cyst hydatid cases treated with surgery.Materials and Methods: The records of 33 patients that were operated on for lung cyst hydatid disease at our clinic between 1999 and 2016 were evaluated retrospectively in terms of demographic data, clinical findings, location of cysts, treatment methods and follow-up.
Results: Among 33 patients included in this clinical analysis study, 20 were male (60.6%) and the mean age was 11.5 (4-15 years). The most common complaint was cough that was observed in 16 patients (48.4%). 78.8% of the patients had only one cyst, whereas 21.2% of the patients had multiple cysts. Cystotomy was performed in 12 patients (36.4%), cystotomy + capitonage in 14 patients (42.4%), and decortication in addition to cystotomy + capitonage in 7 patients (21.2%). There were no postoperative complications and no recurrences were observed during the follow-up.
Conclusions: Surgical treatment is the primary treatment that can be performed successfully and safely in childhood lung cysts hydatids.
Introduction
Hydatid cyst is a parasitic infectious disease that has been known since the time of Hippocrates, caused by Echinococcus granulosus which is commonly found in nature. It is endemic in the Mediterranean countries including Turkey [1-4]. In adults, lung is the second most common localization of the cysts following liver. Whereas in child age group, lungs are at the first rank [2]. Although it is common in adults, children are also frequently affected by this disease [5].In this article, we aimed to present our experience of the surgivcal treatment of lung cyst hydatid at childhood period.
Methods
33 patients under 15 years of age who were operated with the diagnosis of pulmonary hydatid cysts between 1999 and 2016 were retrospectively analysed. Patients" data were obtained from the hospital records. Demographic findings such as age, sex, patients" history and the symptoms and findings determined during physical examination were evaluated. Hematologic and biochemical blood tests, chest X-ray, computed thorax tomography (Thorax CT) and abdominal ultrasonography were performed and the results were reviewed. Localization of cysts, surgical technique and prognosis were evaluated.Results
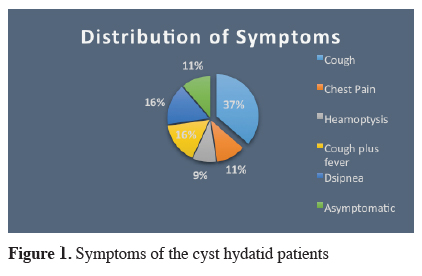
The study was approved by the clinical research ethics committee of Cumhuriyet University (2016-10 / 16). The medical files of 33 cases of hydatid cyst in the pediatric age group were reviewed. 20 of the cases were female (60.6%) and 13 were male (39.4%). The mean age was 11.5 years (within 4-15 years range).Cough was the most common symptom in the majority of cases, whereas 5 cases were asymptomatic. In these 5 patients, the cyst was determined on chest x-ray taken for different reasons. Figure 1 shows the distribution of symptoms.
 Click Here to Zoom |
Figure 1: Symptoms of the cyst hydatid patients |
All patients underwent PA chest X-ray and thorax CT before diagnosis. Except one patient all the patients presented with unilateral cysts. Two (6%) patients had comcomittant liver cysts.
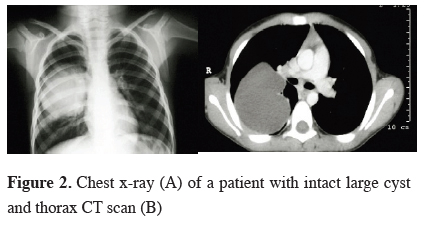
In 26 (78.8%) cases only one cyst was found, where 7 (21.2%) had multiple cysts. The cysts were of equal number in both lungs and lower lobes were more involved (Table 1). In the majority of patients (66.7%) there was a simple single lung cyst and observed as a well defined homogeneous mass in the radiological images (Figure 2). Cyst rupture was detected in 11 patients (33.3%) and no allergic or anaphylactic reaction was reported in any of these patient.
Table 1: Location of the Cyst Hydatid
 Click Here to Zoom |
Figure 2: Chest x-ray (A) of a patient with intact large cyst and thorax CT scan (B) |
All patients underwent a posterolateral thoracotomy. Cystotomy was performed in 12 patients (36.4%), cystotomy + capitonage in 14 patients (42.4%), and decortication in addition to cystotomy + capitonage in 7 patients (21.2%). Decortication had been performed in all cases with perforated hydatid cysts. A parenchymal resection such as lobectomy was not performed in any of the patients. The postoperative course was uneventful and no complications such as prolonged air leak, bronchopleural fistula, abscess or empyema were seen. During the followup no recurrences were detected.
Discussion
Hydatid cyst is an important health problem all over the world and the incidence in our country is 20 / 100.000 [6-10]. Lung is the most frequent location of the hydatid cysts at childhood period [10-12], and its reported that interestingly boys are effected more than girls. The explanation is based on the suggestion that boys start to contact with dogs earlier and more frequent than girls [7,9]. In our study, there was male predominance (60.6%) similar to the literature.Intact lung cysts generally do not cause symptoms and tend to be asymptomatic in pediatric age group. Due to the delay in the diagnosis, the cyst were detected as larger sized cysts [7,13]. In our patient group, the cysts was 5 cm and bigger in diameter in 23 (69.7%) cases.
The patients applied to our clinic with one or more symptoms and cough was the leading one which was reported in 16 (48.4%) patients similar to the reports in the literature [2,10,14].
The most common diagnostic method for lung cyst hydatid disease is chest radiography [14]. The diagnosis of intact or asymptomatic pulmonary hydatid cysts is usually based on suspicion arising from an unexpected finding on routine chest x-ray [5]. Diagnostic radiological imaging methods are accepted to be more reliable than serological tests [8]. Thorax CT is an important imaging modality to demonstrate the density of intact cysts and to detect cysts that are not seen on posteroanterior chest X-ray [5,8].
In the literature it is reported that the pulmonary hydatid cysts are mostly single and multiple occurrence has been reported between 14% and 30%. It is most commonly seen in the lower lobes [7,8,15-17]. In consistent with the literature, 26 (78.8%) of our cases had single cysts and 21 (63.6%) cases had cysts were located at the lower lobes.
The main treatment for lung cyst is surgery [2,7]. The surgeon"s goal is to remove the cyst with the membrane, to eradicate the parasite without forming a contaminant, and to close the remaining cavity [12]. The choice of surgical technique depends on the condition of the tissue surrounding the cyst during surgery. Commonly accepted procedures in surgery are parenchymal protective procedures [7]. While all alive parasitic material is removed, especially in children, the intact lung tissue should be preserved to a maximum extent. The most common surgical method is cystotomy and capitonage [2,18]. In our patients, the most common technique was cystotomy and / or cystotomy + capitonage performed in 32 (96.9%) cases. Especially in children, parenchymal resections should be avoided even if there are complicated cysts as the affected parenchyma in children has a high recovery capacity [2,8]. In our series, no parenchymal resections were performed in any of the patients although the cysts were large or multiple.
It is reported that the most common postoperative complications after cyst surgery are prolonged air leak, pneumonia, recurrence, and empyema (16). In our series, our patients" postoperative follow-up were uneventful and no recurrent disease was observed.
As an alternative to surgery, albendazole therapy has recently been proposed. The efficacy of this treatment is influenced by the thickness of the cyst wall [19]. However, they generally have low response rates, severe drug reactions, markedly high perforations and recurrence rates. For this reason, albendazole therapy should be performed when there is disseminated disease, when the surgery is contraindicated, or in the presence of recurrence risk due to contamination [7]. We only administer albendazole treatment after surgery for the cases having a risk of contamination, as well.
As a conclusion, surgery was performed safely as the primary treatment of pulmonary cyst hydatid in pediatric patients where parenchymal preservation techniques should be preferred.
Declaration of conflicting interests
The author declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The author received no financial support for the research and/or authorship of this article.
Reference
1) Çelik T, Akçora B, Tutanç M, Yetim TD, Karazincir S, Akın MM, et al. Ruptured Pulmonary Hydatid Cyst: a Case Report. Turkiye Parazitol Derg 2012; 36: 45-7.
2) Cangir AK, Sahin E, Enon S, Kavukçu S, Akay H, Okten I, et al. Surgical treatment of pulmonary hydatid cysts in children. J Pediatr Surg 2001; 36: 917-20.
3) Sahin E, Enon S, Cangir AK, Kutlay H, Kavukçu S, Akay H, et al. Single-stage transthoracic approach for right lung and liver hydatid disease. J Thorac Cardiovasc Surg 2003;126: 769-73.
4) Cevik M, Boleken ME, Kurkcuoglu IC, Eser I, Dorterler ME. Pulmonary hydatid disease is difficult recognized in children. Pediatr Surg Int 2014; 30: 737-41.
5) Çelik M, Senol C, Keles M, Halezeroglu S, Urek S, Haciibrahimoglu G, et al. Surgical Treatment of Pulmonary Hydatid Disease in Children: Report of 122 Cases. J Pediatr Surg 35:1710-3.
6) Mahmodlou R, Sepehrvand N, Nasiri M. Saucerization: a modified uncapitonnage method of surgery for pulmonary hydatidosis. World J Surg 2013; 37: 2129-33.
7) Dincer SI, Demir A, Sayar A, Gunluoglu MZ, Kara HV, Gurses A. Surgical treatment of pulmonary hydatid disease: a comparison of children and adults. Journal of Pediatric Surgery 2006; 41: 1230-6.
8) Topcu S, Kurul IC, Tastepe I, Bozkurt D, Gulhan E, Cetin G. Surgical treatment of pulmonary hydatid cysts in children. J Thorac Cariovas Surg 2000; 120: 1097-101.
9) Dakak M, Genc O, Gurkok S, Gözübüyük A, Balkanli K. Surgical treatment for pulmonary hydatidosis (a review of 422 cases). J R Coll Surg Edinb 2002; 47: 689-92.
10) Aydogdu B, Sander S, Demirali O, Guvenc, Besik C, Kuzdan C, et al. Treatment of spontaneous rupture of lung hydatid cysts into a bronchus in children. Journal of Pediatric Surgery 2015; 50: 1481-3.
11) Berberoğlu B, Kaya Z, Aslan A.T, Çelik A, Kurul İ.C, Yücel C. Surgery and Interventional Treatments in a Child with Hydatid Cyst. Gazi Med J 2011; 22: 85-7.
12) Ozdemir A, Bozdemir S.E, Akbiyik D, Daar G, Korkut S, Korkmaz L, et al. Anaphylaxis due to ruptured pulmonary hydatid cyst in a 13-year-old boy. Asia Pac Allergy 2015;5: 128-31.
13) Rebhandl W, Turnbull J, Felberbauer FX, Tasci E, Puig S, Auer H, et al. Pulmonary echinococcosis (hydatidosis) in children: results of surgical treatment. Pediatr Pulmonol 1999; 27: 336-40.
14) Aydın ZGG, Yalcınkaya R, Teke TA, Bayhan GI, Oz FN, Timur OM, et al. Coexistence of Pulmonary Hydatid Cyst and Mycoplasma pneumoniae Pnömonia in a Child. Turkiye Parazitol Derg 2015; 39: 159-63.
15) Koca T, Dereci S, Gencer A, Duman L, Aktaş AR, Akcam M, et al. Cystic Echinococcosis in Childhood: Five-Years of Experience From a Single-Center. Turkiye Parazitol Derg 2016; 40: 26-31.
16) Usluer O, Ceylan KC, Kaya S, Sevinc S, Gursoy S. Surgical management of pulmonary hydatid cysts: is size an important prognostic indicator? Tex Heart Inst J 2010; 37: 429-34.
17) Ekingen G, Tuzlacı A, Güvenç H. Thoracoscopic surgery in the management of pediatric pulmonary hydatid cyst. Turkish J Thorac Cardiovasc Surg 2005; 13: 62-64.



