

2Department of Pathology, Yedikule Chest Diseases and Thoracic Surgery Eduation and Research Hospital, İstanbul, Turkey DOI : 10.26663/cts.2021.0006
Summary
In this report, a case of Hattori’s cyst of Mullerian (HMC) origin, located in the anterior mediastinum is evaluated in light of the literature. A 33-year-old woman presented to our clinic with chest pain. A computed tomography scan of the patient’s thorax revealed a 5x6 cm lesion located on the left paracardiac region. Following the excision of the cyst, a diagnosis of mediastinal HMC was made. Our case shows that cases of MHC, which are rare in the posterior mediastinum, can also be seen in the anterior mediastinum and should be included in the differential diagnosis.Introduction
Primary congenital mediastinal cysts are rare and makeup 10-12% of mediastinal masses [1]. Several types of cysts can be seen in the mediastinum such as thymic, parathyroid, pericardial, neurogenic, bronchogenic, esophageal, and coelomic cysts. However, the most frequently seen type is bronchogenic cysts. When Hattori first identified a mediastinal cyst with Mullerian origin in 2005, he determined that this cyst was lined by ciliated non-stratified cuboidal or columnar epithelium with no cytological atypia [2]. To date, these cysts have been described as rare in the literature. In this report, we evaluate a case of Hattori’s Cyst of Mullerian origin, which we found to be located in the anterior mediastinum, in the light of literature.Case Presentation
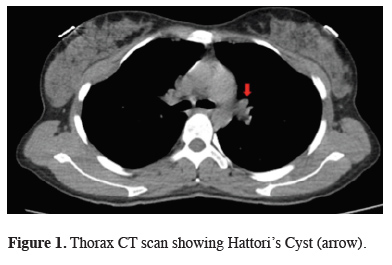
A 33-year-old woman presented to our clinic with non-specific chest pain. She was a non-smoker and had no comorbidities. A CT scan of her thorax revealed a 5x6 cm lesion located on the left paracardiac region (Figure 1).
 Click Here to Zoom |
Figure 1: Thorax CT scan showing Hattori’s Cyst (arrow). |
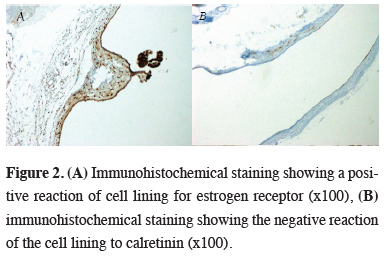
Surgical resection was planned. The patient underwent video-assisted thoracoscopic surgery (VATS). On exploration, a lesion of 5x5 cm, filled with serous fluid, on the left paracardiac region was seen. The cyst showed invasion to the mediastinal pleura; however, it had no invasion to the lungs. Total excision of the cyst was performed. Postoperative histopathological examination showed the cyst wall consisted of smooth muscle and connective tissues lined by ciliated epithelium with no cytological atypia. Immunohistochemical examination showed a positive reaction for Estrogen Receptor (ER) and Wilms’ Tumor Gene 1 (WT-1), and negative for Calretinin (Figures 2a, b). Based on these findings, the patient was diagnosed with Hattori’s Cyst of the mediastinum.
 Click Here to Zoom |
Figure 2: (A) Immunohistochemical staining showing a positive reaction of cell lining for estrogen receptor (x100), (B) immunohistochemical staining showing the negative reaction of the cell lining to calretinin (x100). |
Written informed consent was obtained from the patient for publication of her data.
Discussion
Extra genitourinary tract or pelvic cysts with Mullerian differentiation are rare. They are generally seen in the skin and retroperitoneal cavity in women [3]. Primary congenital mediastinal cysts are rarer and constitute 12-30% of all masses seen in the mediastinum [1]. Hattori found that prior to describing this cyst, mediastinal cysts were misdiagnosed as bronchogenic cysts due to their ciliated epithelium. Thomas-de-Montpreville et al. [3] evaluated 163 consecutive mediastinal non-neoplastic cysts retrospectively and detected cysts conforming to Hattori’s Cyst definition in only 9 cases (5.5%). They underlined that three of these 9 cases were diagnosed with a pleuropericardial cyst at first glance due to the benign cystic nature. Our case was acknowledged to be Hattori’s Cyst, since ER and WT-1 were positive and Calretinin negative.Regarding mediastinal cysts, a decision to operate is frequently made if the patient is symptomatic. As the size of the cyst increases, symptoms (chest pain, shortness of breath, palpitations, coughing, etc.) due to compression increase as well. Follow-up in the outpatient clinics is usually recommended to those patients with asymptomatic, small cysts [4]. Since our patient had symptoms of chest pain, and the cyst was 5 cm, we decided to perform surgery.
To date, 26 cases of Mediastinal Hattori’s Cyst have been published in the literature, including our case. In these cases, the size, location, and symptoms caused by the cyst were investigated, and it was determined that cysts were more common in the left thoracic cavity compared to the right [5].
The cyst of Mullerian origin in the mediastinum is still unclear. The reason for the cysts being at the thoracic location is because of the developmental misplacement of the endosalpingeal or endo-salpingeal epithelium. One theory is that coelomic epithelium develops on the cranial end of the plica mesonephrica at the level of the third to fifth thoracic vertebral blastema [6]. All of the cases published in the literature define the cyst in the posterior mediastinum and paravertebral area. The case we present is the first case of a cyst of embryonic Mullerian origin in the anterior mediastinum.
The prognosis of all cases of Hattori’s Cyst published to date has been shown to be good. Recurrence after surgical resection has not been reported. We performed total excision of the cyst in order to prevent a recurrence. It is difficult to make a preoperative diagnosis; therefore, it is essential that the differential diagnosis of these cysts should be made after resection. This way differentiation of these cystic tumors from bronchogenic or neurogenic cysts can be achieved. Detailed histopathological and immunohistochemical evaluation is imperative for definitive diagnosis.
Previously published 25 cases refer to Hattori’s Cyst in the posterior mediastinum. Our case shows that Hattori’s Cyst can also be seen in the anterior mediastinum and should be included in the differential diagnosis. Further clinical studies are needed to have more information on this subject.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
MSOM; Collected the data, performed the analysis, co-wrote the paper, CBS; performed the analysis, co-wrote the paper, VE, MM; co-wrote the paper, NU; contributed data/analysis tools.
Reference
1) Simmons M, Duckworth LV, Scherer K, Drew P, Rush D. Mullerian cysts of the posterior mediastinum: report of two cases and review of the literature. J Thorac Dis 2013; 5: E8-E10.
2) Hattori H. Ciliated cyst of probable mullerian origin arising in the posterior mediastinum. Virchows Arch 2005; 446: 82-4.
3) Thomas-de-Montpréville V and Dulmet E. Cysts of the posterior mediastinum showing müllerian differentiation (Hattori’s cysts). Ann Diagn Pathol 2007; 11: 417-20.
4) Kocaturk CI, Sezen CB, Aker C, Kalafat CE, Bilen S, Kutluk AC et al. Surgical approach to posterior mediastinal lesions and long-term outcomes. Asian Cardiovasc Thorac Ann 2017; 25: 287-91.



