

2Department of Pathology, Dr. Suat Seren Chest Disease and Thoracic Surgery Training and Research Hospital, İzmir, Turkey DOI : 10.26663/cts.2021.00011
Summary
Background: Bronchogenic cyst is a generally benign and rare congenital anomaly. The mediastinum and lung parenchyma are the most common sites the cysts occur. This study aimed to compare the effectiveness of thoracoscopy and thoracotomy for the treatment of bronchogenic cysts.Materials and Methods: Twenty-one patients were operated on in Dr. Suat Seren Thoracic Surgery Clinic between 2004 and 2019 with the diagnosis of bronchogenic cyst. Patients were divided into two groups according to the surgery method as video-assisted thoracoscopic surgery (VATS) or thoracotomy. Demographic and operative features, radiological findings, and complications were retrospectively analyzed.
Results: Patients underwent either VATS (10 patients) or thoracotomy (11 patients). Sixteen patients underwent simple cyst excision, whereas parenchymal resection was performed for five patients. The mean Visual Analogue Scale (VAS) value was 3.5 ± 1.1 for the VATS group and 6.5 ± 1 for the thoracotomy group. Duration of hospital stay and chest drainage was 4.2 ± 1.7 and 3.2 ± 1.7 days, respectively, in the VATS group, while in the thoracotomy group, it was 7.1 ± 4.5 and 6.1 ± 4.5 days. The time of hospitalization stay, duration of chest drainage, operative time, and VAS values were found statistically significantly lower in the VATS group.
Conclusions: Both VATS and thoracotomy are preferred surgical methods in bronchogenic cyst surgery. VATS is superior to thoracotomy in terms of shorter hospital stay, chest drainage duration, operative time, and lower postoperative pain level. Minimally invasive methods can be chosen safely for the treatment of bronchogenic cyst in appropriate cases.
Introduction
The bronchogenic cyst is a rare congenital anomaly resulting from abnormal branching of the tracheobronchial tree developing from the ventral part of the embryological foregut between the 26th and 40th days of gestation [1]. The bronchogenic cyst is generally located in the middle and posterior mediastinum or lung parenchyma. It is diagnosed incidentally since it is often asymptomatic in adults.Some authors claim conservative treatment for asymptomatic patients. However, video-assisted thoracoscopic surgery (VATS) and thoracotomy are the most preferred treatment options for symptomatic or asymptomatic patients of which can be complicated or developing malignancy. Robotic surgery can also be considered an option in recent years.
In this study, 21 patients operated on with the bronchogenic cyst diagnosis were analyzed in terms of demographic and surgical features. It is aimed to compare the surgical methods accompanied by a literature review.
Methods
Data CollectionThe patients’ records operated in the thoracic surgery clinic of Dr. Suat Seren Chest Diseases and Surgery Hospital between 2004 and 2019 with the diagnosis of mediastinal, parenchymal, or diaphragmatic lesions were reviewed retrospectively. Twenty-one patients whose histopathological diagnosis confirmed as bronchogenic cysts were included in the study. The patients were divided into two groups as those operated by VATS or thoracotomy. The clinical features of these patient groups were reviewed as demographic characteristics at the time of operation (age, gender), preoperative symptoms, anatomical location of the cyst, cyst diameter, operative method, chest tube drainage duration, postoperative hospital stay, postoperative complications, and recurrence. All patients underwent routine blood tests, posteroanterior (PA) and lateral chest X-ray, and thorax computed tomography (CT) preoperatively. Magnetic resonance imaging (MRI) is used for determining the nature of the cyst. The study was approved by the institutional review board (No: 2019/5.1) and conducted per the principles of the Declaration of Helsinki.
Operation Method
Following the double-lumen intubation, all patients were operated on in the right or left lateral decubitus position. One of the patients with a mediastinal bronchogenic cyst of subcarinal position was operated in the supine position. As the operation method, thoracotomy was performed before 2010, whereas VATS was preferred for suitable cases after this year. Depending on the cyst’s anatomical location, fourth or fifth intercostal space was used for thoracotomy. In the VATS approach, a utility incision (4th or fifth intercostal space) and a camera port of length 1 cm on the sixth or seventh intercostal space of the midaxillary line were used. The absence of air leakage for at least 24 hours and pleural drainage less than 200 mL per day were considered as the criteria to remove the chest tube. The air leakage that lasted seven days or more was considered as prolonged air leakage. The patients’ postoperative pain level was determined according to the subjective assessment method of the Visual Analogue Scale (VAS).
Statistical Analysis
Statistical Package for the Social Sciences (SPSS) version 22.0 program was used to analyze data. Continuous data were specified as mean ± standard deviation, and median (minimum-maximum) values. Mann-Whitney U test was used to compare differences between groups and Fisher’s Exact test for dichotomous variables. A p-value less than 0.05 was considered as statistically significant.
Results
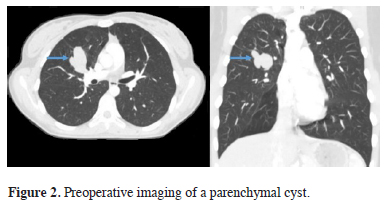
The mean age of 11 female and ten male patients was 41.3 ± 18.6 years (18-78). Eighteen of the patients (85%) were asymptomatic consistent with the literature. Fever, chest pain, dyspnea, cough were the complaints of symptomatic patients. All the patients underwent a thorax CT. MRI was also used for eight patients in which the nature of the cyst could not be clearly identified. MRI confirmed all the lesions as cyst successfully. Radiological imaging examples of mediastinal and parenchymal cysts are presented as figures 1 and 2.
 Click Here to Zoom |
Figure 1: Preoperative imaging of a mediastinal cyst. |
 Click Here to Zoom |
Figure 2: Preoperative imaging of a parenchymal cyst. |
The median cyst diameter was 4.5 cm (1-10). None of the cysts had any tracheobronchial connection. Comparative characteristics of patients who underwent VATS and thoracotomy are summarized in table 1.
Table 1: The characteristics of patients who underwent VATS and thoracotomy.
Patients underwent either thoracotomy (11 patients) or VATS (10 patients). Simple cyst excision (16 patients), wedge resection (3 patients), lobectomy (1 patient), and lobectomy and segmentectomy (1 patient) were the surgical procedures performed. The anatomical localization of the cyst is presented in table 2. A bronchial laceration was repaired in one patient intraoperatively, and that patient's bronchial system was observed to be intact by bronchoscopy in the postoperative period. Five patients had prolonged air leakage as the postoperative complication (23%). The median duration of postoperative hospitalization was 6 days (2-19). VATS patients’ hospital stay duration (p = 0.03), drainage duration (p = 0.03), operative time (p = 0.013), and VAS score (p < 0.001) of the patients operated by VATS were found to be statistically significantly lower than thoracotomy group. There was no statistically significant difference between the two groups regarding age, gender, cyst diameter, and postoperative complications. No recurrence was observed in any of the patients during the median follow-up of 94.5 months (15-190).
Discussion
The bronchogenic cyst is a rare, benign lesion that arises from abnormal budding of the tracheobronchial tree. The most commonly affected site is mediastinum, but the location may be parenchymal in 15-20% of the cases [2]. It is mainly located in the paratracheal and subcarinal regions of the mediastinum. Although mediastinum and parenchyma are the primary localizations, they may be seen on ectopic locations such as retroperitoneum, neck, cranial fossa, pericardium [3,4]. The majority of the patients in our study (71%) had mediastinal cysts, and most of them were located at the paratracheal region, similar to the literature review. Besides, the cyst was observed on the diaphragm in one patient.The clinical manifestations may vary, and the cysts are usually asymptomatic in adults until they reach large sizes and compress other structures or be infected due to having a bronchial connection. The most common symptoms are chest pain, cough, dyspnea, dysphagia, hemoptysis, depending on compression and location of the cyst [5]. Also, it has been reported in the literature that they may cause arrhythmia due to cardiac pressure when they reach large dimensions [6]. Several studies reported that the majority of asymptomatic patients will develop symptoms over time [7]. Only three (14%) patients had symptoms in our series, all located in the pulmonary parenchyma. Fever, chest pain, cough, and dyspnea were the complaints of symptomatic patients, consistent with the literature.
Preoperative diagnosis of bronchogenic cysts may be challenging due to having a wide range of radiological and clinical features. Thoracic computed tomography (CT) and magnetic resonance imaging (MRI) have an essential value in determining the size, shape, content, and relationship of the cyst with surrounding tissues [8]. Attenuation coefficient or Hounsfield Unit (HU) value on CT can be a marker to determine the lesions as solid or cystic [9]. While cyst at mediastinum localization is generally presented as well-defined masses, the air-fluid level is the radiological finding of parenchymal cysts connected with bronchi. In case of infection, higher HU values can be obtained on CT due to protein and calcium within the cyst in contrast to low HU like water or soft tissue of cystic lesions. Higher HU may be evaluated in favor of semisolid or solid masses. MRI provides more valuable information than CT when solid or cystic lesions cannot be differentiated [11]. The median and mean HU values were obtained as 34 (10-90) and 39 ± 20.7, respectively, in our study. This value was higher than the water density and 20 HU in which was evaluated in favor of a cyst. This result may be related to the proteinous content in the cyst. Cases of bronchogenic cysts with high HU values have been reported in the literature similarly to our study [11].
The primary treatment for symptomatic or complicated cases is surgery to relieve symptoms and prevent complications such as infection and compression. However, on the other hand, there is still no consensus regarding the management of asymptomatic patients. Wang et al. suggested that a conservative approach may be appropriate provided that radiological follow-up is performed for this group of patients since the malignant transformation is not very frequent in asymptomatic patients [12]. On the other hand, opposite opinions have claimed that surgery should be performed instead of conservative treatment [13] since adenocarcinoma may arise from bronchogenic cyst [14]. Surgery was performed for 18 patients in our study, even if they had no symptoms, considering the possibility of developing malignant degeneration and symptoms over time. As we did not follow up asymptomatic patients conservatively, we do not have sufficient data on long-term outcomes of non-operated asymptomatic patients. We favor surgery for patients even though they are asymptomatic since the malignant transformation is a possibility. Although conservative treatment may be an option for elderly asymptomatic patients, thoracotomy was performed on a 78-year-old symptomatic male patient to relieve his symptoms in our study.
The appropriate treatment approach is the complete removal of the lesion for mediastinal cysts and anatomical or wedge resection for parenchymal cysts. Wedge resection is adequate for small-sized peripheral parenchymal lesions. Lobectomy should be chosen for centrally located parenchymal lesions. While lobectomy is usually performed as anatomical resection, segmentectomy may also be preferred in appropriate cases. Segmentectomy can be performed if the cyst does not exceed the boundary of the segment of the involved lobe. In our study, simple cyst excision was performed for mediastinal and diaphragmatic cysts, while patients with parenchymal cysts underwent pulmonary resection.
Complete removal of the cyst should be the primary goal since recurrence in postoperative follow-up may occur in a cyst that has not been excised totally [15]. However, adhesions with major structures may prevent complete excision of the cyst, especially in infected patients. In this case, destruction of the mucosal layer of the cyst by using electrocautery is suggested to prevent recurrence [16]. According to Fievet et al [17], early excision of the cyst between the 6th and 12th month of life could prevent surgical complications and incomplete cyst excision, eliminating the need for electrocautery use.
The cyst was totally excised in all patients of our study. No recurrence was obtained in any patient during the median follow-up of 94.5 months (15-190).
The preferred surgical approaches are generally VATS and thoracotomy. Duration of chest drainage for the VATS group is reported to be shorter than thoracotomy group in the literature [18]. In addition, the VATS group is superior to thoracotomy in terms of shorter operative time, shorter postoperative hospital stay, and less intraoperative blood loss [19]. When comparing VATS and thoracotomy groups in our study, the VATS patients had statistically significant shorter hospital stay, shorter operative time, lower VAS scores, and shorter chest drainage duration (p < 0.05). VATS clearly has advantages, including low pain severity and good exposure to the thoracic cavity compared to thoracotomy [20].
Adhesions due to infection can lead to complications, especially in symptomatic patients. One patient with a mediastinal cyst located on the subcarinal region suffered an iatrogenic injury of the bronchus in our series, similar to Granoto et al, who reported bronchus injury on two patients due to sharp dissection for adhesions of mediastinal cysts [21]. The bronchial laceration was repaired intraoperatively by thoracotomy before the patient was discharged without any other complication in the postoperative period. Besides, a prolonged air leak was observed in five patients.
Since adhesions due to infection sometimes make the thoracoscopic approach difficult, a thoracotomy may be needed. At this point, robotic surgery can be considered an alternative to thoracotomy in the advantages of 3D image quality and the manoeuvrability of the instruments used [22].
Today, bronchogenic cyst operation, with the development of thoracoscopic surgery, is performed safely in a minimally invasive manner, and patients are discharged in a short time without any severe complications.
In conclusion, surgery should be performed to both confirm the diagnosis and prevent complications and malignant transformations. Since videothoracoscopy is superior to conventional thoracotomy in the ways of shorter hospital stay, shorter chest drainage duration, shorter operative time, and lower VAS score, minimally invasive methods can be chosen safely as the first choice for the treatment of bronchogenic cyst in appropriate cases.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics Approval
The study was approved by the Ethics Committee of University of Health Sciences, Dr. Suat Seren Chest Disease and Thoracic Surgery Training and Research Hospital (No: 2019/5.1) and conducted in accordance with the principles of the Declaration of Helsinki.
Authors’ contributions
HM; Collected the data, co-wrote the paper, conceived and designed the analysis, KCC; Co-wrote the paper, performed the analysis, ŞÖK; Contributed data or analysis tools, AGY: Contributed data or analysis tools.
Reference
1) Kiralj A, Vučković N, Mijatov I. Congenital cervical bronchogenic cyst: a case report. Srp Arh Celok Lek 2015; 143: 317-21.
2) Parray FQ, Sherwani AY, Dangroo SA, Bisati RA, Malik NS. Retroperitoneal bronchogenic cyst mimicking hydatid liver: a case report. Case Rep Surg 2012; 2012: 312147. doi: 10.1155/2012/312147.
3) Goswamy J, De Kruijf S, Humphrey G, Rothera M, Bruce I. Bronchogenic cysts as a cause of infantile stridor: case report and literature review. J Laryngol Otol 2011; 125: 1094-97.
4) Castro R, Oliveira M, Fernandes T, Madureira A. Retroperitoneal bronchogenic cyst: MRI findings. Case Rep Radiol 2013; 2013: 853795. doi: 10.1155/2013/853795.
5) Caterino U, Amore D, Cicalese M, Curcio C. Anterior bronchogenic mediastinal cyst as priority procedure for robotic thoracic surgery. J Thorac Dis 2017; 9: E674.
6) Smail H, Baste JM, Melki J, Peillon C. Mediastinal bronchogenic cyst with acute cardiac dysfunction: two-stage surgical approach. Ann Thorac Surg 2015; 100: e79-e80.
7) Patel SR, Meeker DP, Biscotti CV, Kirby TJ, Rice TW. Presentation and management of bronchogenic cysts in the adult. Chest 1994; 106: 79-85.
8) Panchanatheeswaran K, Dutta R, Singh KI, Kumar A. Eleven-year experience in thoracoscopic excision of bronchogenic cyst. Asian Cardiovasc Thorac Ann 2012; 20: 570-4.
9) Mendelson DS, Rose JS, Efremidis S, Kirschner P, Cohen BA. Bronchogenic cysts with high CT numbers. AJR Am J Roentgenol 1983; 140: 463-5.
10) McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, Matsumoto S. Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology 2000; 217: 441-6.
11) Vos CG, Hartemink KJ, Golding RP, Oosterhuis JWA, Paul MA. Bronchogenic cysts in adults: frequently mistaken for a solid mass on computed tomography. Wien Klin Wochenschr 2011; 123: 179-82.
12) Wang X, Chen K, Li Y, Yang F, Zhao H, Wang J. The video-assisted thoracic surgery for mediastinal bronchogenic cysts: a single-center experience. World J Surg 2018; 42: 3638-45.
13) Jung HS, Kim DK, Lee GD, Sim HJ, Choi SH, Kim HR et al. Video-assisted thoracic surgery for bronchogenic cysts: is this the surgical approach of choice? Interact Cardiovasc Thorac Surg 2014; 19: 824-9.
14) Endo C, Imai T, Nakagawa H, Ebina A, Kaimori M. Bronchioloalveolar carcinoma arising in a bronchogenic cyst. Ann Thorac Surg 2000; 69: 933-5.
15) Hasegawa T, Murayama F, Endo S, Sohara Y. Recurrent bronchogenic cyst 15 years after incomplete excision. Interact Cardiovasc Thorac Surg 2003; 2: 685-7.
16) Weber T, Roth TC, Beshay M, Herrmann P, Stein R, Schmid RA. Video-assisted thoracoscopic surgery of mediastinal bronchogenic cysts in adults: a single-center experience. Ann Thorac Surg 2004; 78: 987-91.
17) Fievet L, D’Journo XB, Guys JM, Thomas PA, De Lagausie P. Bronchogenic cyst: best time for surgery? Ann Thorac Surg 2012; 94: 1695-9.
18) Tölg C, Abelin K, Laudenbach V, De Heaulme O, Dorgeret S, Lipsyc ES et al. Open vs thorascopic surgical management of bronchogenic cysts. Surg Endosc 2005; 19: 77-80.
19) Guo C, Mei J, Liu C, Deng S, Pu Q, Lin F et al. Video-assisted thoracic surgery compared with posterolateral thoracotomy for mediastinal bronchogenic cysts in adult patients. J Thorac Dis 2016; 8: 2504.
20) Amore D, Cerqua FS, Perrotta F, Cennamo A, Curcio C. Bilateral simultaneous VATS for complete resection of bilateral posterior mediastinal bronchogenic cyst: a case report. Int J Surg Case Rep 2016; 28: 149-51.



