

2Department of Pathology, Izmir Dr. Suat Seren Chest Diseases and Thoracic Surgery Training and Research Hospital, Izmir, Turkey DOI : 10.26663/cts.2017.0004
Summary
Background: Solitary fibrous tumors (SFT) are rare seen tumors assessed to be originated from pleura. Even though they are benign, after their complete resections malignant recurrences might be seen in follow up period. In this study, based on our case series undergone complete surgical resection due to SFT, we looked for an answer whether if it is convenient to accept these tumors as benign or not.Materials and Methods: Patients undergone surgery between January 2000 and January 2011 were included in this study. Follow up data, patients and tumor histopathological characteristics were analysed.
Results: Our series consisted of 14 cases (eight male, six female) with a mean age of 49.5 ± 15.3 (15-70 years). All patients" undergone thoracotomy, and complete resection was performed. The mean follow-up was 50.3 ± 30.6 months (between 9 -101 months). Two recurrences were detected and both patients died due to recurrent disease.
Conclusions: Though they are considered to be benign lesions, SFT have a potential to come along with malignant recurrences. Recurrences were observed in giant tumors and this makes us think if it is possible to overlook a malignant focus in histopathological observation in such kind of big tumors. In this sense, patients should be informed in this regard and a complete and wide resection should be performed as much as possible with a long time follow up period as malignant diseases.
Introduction
Solitary fibrous tumors are mesenchymal tumors considered to be a form of mesothelioma and named as "benign pleural lipoma, localized pleural mesothelioma" in the past decades. They might origin from parietal or visceral pleura [1]. Since it has been first described in 1937, been the subject of several literature due to its rarity.Although most of the patients are asymptomatic, nonspecific symptoms such as chest pain, shortness of breath and cough might be seen [2-7]. Because sometimes preoperative diagnosis have difficulties, complete resection is necessary for definitive diagnosis and treatment.
As we are going to discuss in this study, because of the potential for malignant recurrence following up the patients is also as important as complete resection. The aim of this study is to shed light on these points in the evaluation of our operated patients.
Methods
Patients undergone surgery between January 2000 and January 2011 in our department consecutively and diagnosed as a solitary fibrous tumor histopathologically were included in this study. We declare that the study was performed in accordance with the ethical standards laid down in the Helsinki Declaration of 1975, as revised in 1983. Routine laboratory tests, respiratory function tests, chest X-ray and thorax computed tomography (CT) were done for all preoperative patients. The limitation of pulmonary function tests, in patients with a large lesion size, did not affect our surgical decision. Positron emission tomography was performed in only 2 patients demonstrating benign lesions with low FDG uptake. Patients with suspected invasion of surrounding tissues were evaluated with thoracic magnetic resonance imaging (MRI). Patients with no evidence of a significant invasion were operated after informed consent was taken. When any association with visceral pleura was detected, safe surgical margins were obtained with wedge resection. Similarly for the parietal pleura, care was taken to perform a wide resection to obtain safe surgical margins. These margins were all proved via frozen section analysis. Histopathological classification was done due to England criteria. Patients were analysed retrospectively according to age, sex, symptoms, radiologic features, preoperative diagnosis, type of operation, postoperative diagnosis and survival.Results
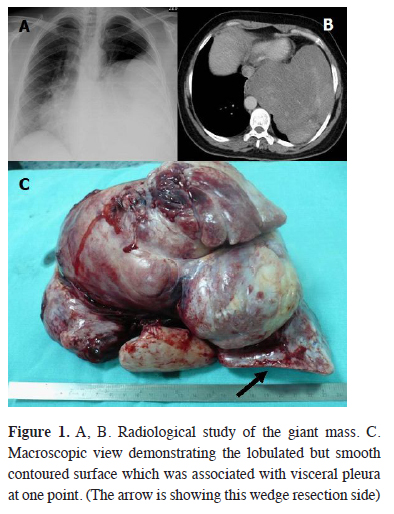
The mean age of the 14 patients included in the study was 49.5 ± 15.3 years (range 15-70 years). Eight patients were male and six were female. While two of the patients were asymptomatic, other were suffering from chest pain, shortness of breath, cough and sputum in the order of frequency. The location of the lesions were the same for right and left hemithorax. The median tumor size was 11.7 ± 6.6 cm (range: 2.5-24 cm) when six of them were larger than 15 cm (Figure 1).
 Click Here to Zoom |
Figure 1: A, B. Radiological study of the giant mass. C. Macroscopic view demonstrating the lobulated but smooth contoured surface which was associated with visceral pleura at one point. (The arrow is showing this wedge resection side) |
Preoperative diagnosis was obtained in a limited number of the patients, while some were diagnosed as "spindle cell mesenchymal tumor" and some were reported as "nondiagnostic material". All patients undergone thoracotomy. Complete resection was intended, so tumors associated with parietal pleura were resected with surrounding parietal pleura, and for those associated with visceral pleura wedge resection was performed (in 12 patients) including tumor free parenchymal lung tissue. Tumors were originating from visceral pleura in eight cases, parietal pleura in two and from both pleura in four cases.
Median follow up time was 50.3 ± 30.6 months (range 9-101 months) and was done with physical examination, chest X-ray and CT. One of the patients was reoperated in the 8th month of her follow up due to recurrent gigantic mass. The first operation specimen was reported as "benign" at histopathological analysis and immunohistochemical analysis revealed vimentin (+) while it was pancytoceratine (-) (Figure 2). At the second exploration because of the extensive invasion to peripheral tissue, resection was not possible and the mass was reported as "sarcoma". Both of the patient"s pathological materials were reviewed retrospectively again in our pathology department and another reference hospital. The patient died in the 9th month of her follow up.
 Click Here to Zoom |
Figure 2: A, B. Imaging of the compressive gigantic mass. C. The lobulated solid tumor weighed 2.5 kg, measured 20x11x6 cm. D. Monotonous spindle cells in the form of a myxoid stroma without cellular atypia, necrosis and mitosis (HEx200) E. Immunohistochemical vimentin (+) stain. |
Another patient was reoperated due to recurrence in 3rd year. The same patient had recurrence suspected to have invasion to surrounding tissue in the 7th year of her follow up and refused any treatment. This recurrence contributed to her death 101 months after the initial operation. Both tumors were larger than 15 cm. in the two patients with recurrence. Other 12 patients were all disease free in their follow up. Patients" demographic data is in Table 1.
Table 1: Clinical and pathological features of the 14 patients
Discussion
Solitary fibrous tumors take place in the literature due to their rarity and the difficulties in both diagnosis and treatment. According to large series majority of the patients are between 40-60 years [3,5]. The major series reported recently are shown in Table 2.Table 2: Data of the large series from literature
In terms of gender although in our series sex distribution seems to be equal, Guo et al. [3] reported the rate of female/male as 2.25. Median age was 44.6 in the same series where as it was 49.5 in our study group.
Preoperative respiratory function tests might be at the border or lower than expected especially in patients having gigantic solitary fibrous tumors. This condition might be due to the compression of the tumor to the lung, so it should be taken into consideration that the patient might have better postoperative FEV1 results [8].
Thorax CT and if necessary MRI, can be used for diagnosis except for chest X-ray and routine tests [2-4,9]. There is not a definitive radiological sign defined for differentiating benign and malignant tumors. Nonetheless heterogeneity, mass effect and pleural effusion are more frequent in malignant solitary fibrous tumors [10]. In addition it is reported that positron emission tomography have limited diagnostic value in solitary fibrous tumors [11,12].
It is generally difficult to have a diagnosis at the preoperative period in SFT, most of the patients have their definitive diagnosis at the postoperative period. Orki et al. [13] reported their three patients, two of whom did not have diagnostic findings although their preoperative biopsy. Similarly, Guo et al. [3] reported the limited assistance of preoperative biopsy for the diagnosis, emphasizing the risk of tumor seeding and avoiding unnecessary biopsies [14]. Compatible with the literature, our patients had their definitive histopathological diagnosis with surgical resection [3,6,7,13]. Chu et al. [4], emphasized that puncture biopsy is a valuable tool for diagnosing SFT, and added that the key is obtaining a sufficient amount of biopsy tissue for successful immunohistochemical staining.
Although in our study all patients postoperative pathological evaluation was reported to be benign, it seems that the rate of malignancy mentioned in the literature, is higher than expected. At the study of Lu et al. [2] seven of the cases from 13, were diagnosed to be malignant. Among them, one patient experienced a recurrence and one patient died of brain metastasis. According to data from this study and our study, the behavior of the tumor is more important than it is histopathological analysis such as benign or malignant. A solitary fibrous tumor which is considered to be benign, may show a malignant progress with malignant recurrences. At this point a question comes into mind: whether is it possible to overlook a malignant focus in the large sized tumors at the histopathological evaluation? A correlation between malignancy and tumor size is investigated. However, in our series, six cases having tumors larger than 15 cm. were all reported as benign. In clinical follow up, in two of these cases recurrence and malignancy was detected, and both of them died without having the chance of any intervention. It should be kept in mind that with the tumor size getting bigger the risk of having a malignant focus inside is more possible and the risk of overlook is more conceivably. Although there are studies supporting our data at this point [3], there are also those who argue the opposite [5,7].
In the study of Guo et al. [3] 10.3% of the patients were detected to be malignant from 39. One patient had recurrence at the 6th month of his follow up, but refused further treatment as the case in our study who had recurrence at the 8th month. The rate of malignancy was similar in the series of Harrison-Phipps et al. [5] (13%), and were detected at the ones having malignant solitary fibrous tumors. Ultimately 75% of the patients with malignant SFTs and 25% patients with benign SFTs experienced recurrence. All of them had re-resection. Five year survival rates were statistically different (89% vs 45.5%, P = 0.0005). Lahon et al. [7] reported a five year survival rate of 96% in the group with benign SFTs, whereas this rate decreases to 68% in malignant ones (P = 0.0003).
In the management of solitary fibrous tumors it is considered to be very important to make a complete surgical resection. To prevent recurrences, getting safe surgical margins with performing a wedge resection for the tumors arising from visceral pleura and associated with lung parenchyma is fundamental [3,9]. It was necessary to perform wedge resection to 12 of the patients in our study. If the tumor grows into the parenchymal tissue lobectomy also might be required [3,4,9].
In conclusion, although solitary fibrous tumors are considered to be benign tumors, it is very important for the surgeons to perform a complete resection to prevent recurrence. Recurrences detected during follow up period seem like as a result of malignant potential. We are in the opinion that, taking into account of this possibility, the objective of the pathologist should be observing the whole material cautiously not to overlook a tumor foci in a side of a gigantic mass. Also based on this possibility, surgeons should follow up their patients for a long time.
Declaration of conflicting interests
The author declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The author received no financial support for the research and/or authorship of this article.
Reference
1) Shields TW, Yeldandi AV. Localized fibrous tumors of the pleura. In: Shields TW, LoCicero III J, Ponn RB, Rusch VW, eds. General Thoracic Surgery. Philadelphia: Lippincot Williams & Wilkins, 2005:889-900.
2) Lu C, Ji Y, Shan F, Guo W, Ding J, Ge D. Solitary fibrous tumor of the pleura: an analysis of 13 cases. World J Surg 2008; 32: 1663-8.
3) Guo W, Xiao HL, Jiang YG, Wang RW, Zhao YP, Ma Z, et al. Retrospective analysis for thirty-nine patients with solitary fibrous tumor of pleura and review of the literature. World J Surg Oncol 2011; 9: 134-9.
4) Chu X, Zhang L, Xue Z, Ren Z, Sun Y, Wang M, et al. Solitary fibrous tumor of the pleura: An analysis of forty patients. J Thorac Dis 2012; 4: 146-154.
5) Harrison-Phipps KM, Nichols FC, Schleck CD, Deschamps C, Cassivi SD, Schipper PH, et al. Solitary fibrous tumors of the pleura: results of surgical treatment and long-term prognosis. J Thorac Cardiovasc Surg 2009; 138: 19-25.
6) Orki A, Eryigit H, Akin O, Patlakoglu S, Kosar A, Haciibrahimoglu G, et al. Plevranın soliter fibröz tümörleri. Fırat Tıp Dergisi 2007; 12: 197-200.
7) Lahon B, Mercier O, Fadel E, Ghigna MR, Petkova B, Mussot S, et al. Solitary fibrous tumor of the pleura: outcomes of 157 complete resections in a single center. Ann Thorac Surg 2012; 94: 394-400.
8) Furukawa N, Hansky B, Niedermeyer J, Gummert J, Renner A. A silent gigantic solitary fibrous tumor of the pleura: case report. Journal of Cardiothoracic Surgery 2011; 6: 122-5.
9) Guo J, Chu X, Sun YE, Zhang L, Zhou N. Giant solitary fibrous tumor of the pleura: an analysis of five patients. World J Surg 2010; 34: 2553-7.
10) Walid Abu Arab. Solitary fibrous tumours of the pleura. Eur J Cardiothorac Surg 2012; 41: 587-97.
11) Cardinale L, Ardissone F, Garetto I, Marci V, Volpicelli G, Solitro F, et al. Imaging of benign solitary fibrous tumor of the pleura: a pictorial essay. Rare Tumors 2010; 2: e1.
12) Ginat DT, Bokhari A, Bhatt S, Dogra V. Imaging features of solitary fibrous tumors. AJR 2011; 196: 487-95.



