

2Department of Internal Medicine, Ege University, School of Medicine, Izmir, Turkey
3Department of Thoracic Surgery, Ege University, School of Medicine, Izmir, Turkey DOI : 10.26663/cts.2021.0016
Summary
Acute mediastinitis is an infection of the mediastinal tissue, which is a rare condition with high mortality and morbidity usually requiring intensive care follow-up. The most common reported causes of this condition are postoperative mediastinitis and descending necrotizing mediastinitis. The patients of the condition usually present with nonspecific symptoms such as fever, dysphagia, and chest pain. Laboratory findings observed are nonspecific, and also leukocytosis and high C reactive protein (CRP) values are encountered. Heterogeneity in the mediastinal tissues, air densities in the mediastinum and loculated fluid collections are radiologically observed. The treatment of the condition is antibiotherapy and surgery. Hemothorax is not reported as an expected complication in the follow-up of mediastinitis. In this case report, we present a patient with hemothorax hospitalized with the diagnosis of mediastinitis and empyema after an extraction of a tooth.Introduction
Acute mediastinitis is an infection of the mediastinal and surrounding connective tissues with an incidence rate of 0.3-5% causing high mortality as it affects such vital organs as the heart, large vessels, trachea and bronchi. Postoperative mediastinitis, descending necrotizing mediastinitis (DNM) and fibrous mediastinitis are the leading causes in etiology, of these, postoperative mediastinitis and DNM often have an acute and fulminant course, whereas fibrous mediastinitis follows a chronic and asymptomatic course. Staphylococcus aureus is the most common cause of postoperative mediastinitis with a rate of 60-80%. DNM is generally polymicrobial as it develops as a result of the spread of pharyngeal or odontogenic infection [1].Hemothorax is the presence of blood in the pleural space caused mostly by trauma. Non-traumatic hemothorax causes are less common which can be listed as malignancy, anticoagulants, vascular ruptures (aortic dissection, arteriovenous malformation), endometriosis, and vascular adhesions in spontaneous pneumothorax [2].
In this study, a case report of a descending necrotizing mediastinitis developing after tooth extraction and resulting in hemothorax is presented.
Case Presentation
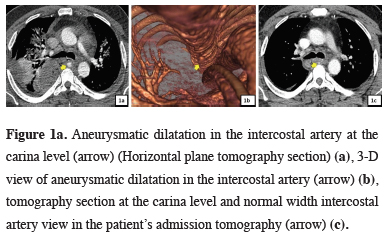
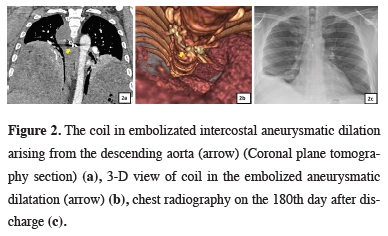
A 35-year-old male patient, who had a history of tooth extraction about two months ago, was admitted to the emergency department with the complaints of dyspnea, rash on the neck and chest skin accompanied by pain. The patient was present with no comorbidities except for diabetes mellitus. In his physical examination, respiratory sounds could not be heard in the basal lung zones. Blood pressure was 130/80 mmHg, pulse 92/min, body temperature was 38.3˚C, and respiratory rate was 14/min. In the first laboratory results, leukocytosis and increased CRP were detected. Pleural effusion in bilateral lower zones was detected in the chest radiography of the patient and the mediastinum was wider than normal. Computed tomography (CT) revealed abscess formation in the retropharyngeal area, heterogeneous opacities in the mediastinum and bilateral pleural effusion. Bilateral chest tube was inserted, and bilateral empyema fluid was drained. Ceftriaxone and metronidazole were started as empirical treatment. No bacterial signal was detected in pleural fluid microbiological examination. In the follow-up of the patient, the pulse rate increased to 130/min, respiratory rate to 20/min, while blood pressure decreased to 80/50 mmHg. Due to worsening clinical findings, he was taken to the intensive care unit with a pre-diagnosis of systemic inflammatory response syndrome (SIRS). Antibiotherapy was changed to piperacillin-tazobactam and teicoplanin and 1 g/kg/day intravenous immunoglobulin was added to the treatment. Staphylococcus hominis and staphylococcus haemolyticus were detected in blood culture. No evidence of immunodeficiency was found in the patient’s tests. It was thought that the retropharyngeal abscess progressed to mediastinitis due to poorly controlled diabetes. On the 10th day of the treatment of the patient whose SIRS findings regressed, postprandial hemoptysis and hypovolemic shock developed. Hemorrhagic drainage was started from the thoracic drain. There was hemothorax in the right hemithorax on thoracic tomography. When the images were examined in detail, an intercostal artery aneurysm (Figures 1a,b) showing active extravasation originating from the descending aorta and crossing the esophagus towards the right hemithorax was detected. Aneurysmatic intercostal artery was embolized (Figures 2a,b). The thoracic drain of the patient, whose infection regressed and hemorrhagic drainage was ended, was removed after embolization. The patient was discharged on the 32nd day of the treatment. Pleural decortication was planned when the pulmonary capacity was found to be decreased in the polyclinic control. Pleural decortication was applied to right hemithorax on the 30th day and to left hemithorax on the 120th day following the discharge. The patient was evaluated with chest radiography (Figure 2c) and respiratory function test on the 180th day. The forced expiratory volume (FEV1), which was 1620 mL in the preoperative pulmonary function test, increased to 2290 mL in the postoperative 6th month.
 Click Here to Zoom |
Figure 1a: Aneurysmatic dilatation in the intercostal artery at the carina level (arrow) (Horizontal plane tomography section) (a), 3-D view of aneurysmatic dilatation in the intercostal artery (arrow) (b), tomography section at the carina level and normal width intercostal artery view in the patient’s admission tomography (arrow) (c). |
 Click Here to Zoom |
Figure 2: The coil in embolizated intercostal aneurysmatic dilation arising from the descending aorta (arrow) (Coronal plane tomography section) (a), 3-D view of coil in the embolized aneurysmatic dilatation (arrow) (b), chest radiography on the 180th day after discharge (c). |
Written informed consent was obtained from the patient for publication of his data.
Discussion
Descending mediastinitis is a rare disease that can be progressive and life threatening. It usually develops after dental infections (36-47%). The other causes are pharyngeal infections and head and neck infections. Patients usually present with symptoms such as fever, skin rash and warmth and pain. In advanced cases, crepitation may develop in the skin of the affected area [3]. Our patient in this case presented with chest pain, rash on the neck and anterior chest wall skin in compliance with the literature. When the patient with poor oral hygiene was questioned, it was learned that he had a history of tooth extraction 2 months ago.CT may be preferred for detailed imaging in patients with suspected mediastinitis learning the patient’s history and conducting the physical examination. On CT scans, loculated mediastinal fluid, mediastinal air densities, decreased adipose tissue density, pleural-pericardial effusion, and mediastinal lymphadenopathies are significant findings in terms of mediastinitis [4]. When our case was evaluated with CT, heterogeneity in the mediastinal tissues, bilateral pleural effusion and retropharyngeal abscess were detected. For this reason, the patient who underwent bilateral tube thoracostomy was diagnosed with empyema secondary to descending mediastinum. He was taken to the intensive care unit due to worsening vital signs and development of SIRS.
Despite the drainage, use of antibiotics and advances in intensive care treatment, the mortality rate caused by oropharyngeal and dental deep neck infections is still high. Delay in diagnosis and treatment of deep neck infection may end up with descending necrotizing mediastinitis. According to the literature, the mortality rate associated with descending mediastinitis before the introduction of aggressive surgical debridement techniques was 40-50%. The reason for this high mortality rate was associated with the fact that descending mediastinitis continues the infective process, causing empyema, pleural and pericardial effusion, pericarditis and blood vessel erosion. In severe mediastinitis, the mortality rate can rise up to 67%. There are many surgical approaches such as cervicotomy, thoracotomy, mediastinotomy or lavage through the thoracic drain [5]. We preferred to insert bilateral chest drain and daily pleural lavage because the purulent fluid was drained into both hemithorax in our case.
The patient who developed acute hemorrhagic drainage from the thoracic drain was evaluated with CT in terms of possible causes of hemorrhage. Interestingly, an aneurysmal dilatation was observed in intercostal artery originating from the aorta and extending towards the right hemithorax at the level of the tracheal bifurcation. When the previous tomography sections of the patient were examined, it was found that this aneurysm was not present on his admission imaging and that the intercostal arteries at the bifurcation level were normal. Intercostal artery aneurysm was urgently embolized. Hemorrhagic drainage from the thoracic drain ended in approximately 1 hour. The patient, who survived the acute empyema period, was applied pleural decortication in the chronic period because of empyema-related pleural thickening and decreased respiratory capacity.
In conclusion, this mediastinitis case which seems to be classical in terms of etiology, symptoms and laboratory results has drawn an interesting path due to the aneurysmatic dilatation of the intercostal artery. This case showed us that hemothorax should be kept in mind as an important cause of mortality in patients with mediastinitis. We are of the opinion that our report will contribute to the literature in terms of both mediastinitis resulting in postprandial hemothorax and the management of this emergency.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
SA, ŞMKB, TİA, DB; Collected the data, performed the analysis, co-wrote the paper.
Reference
1) Kappus S, King O. Mediastinitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-.Available from: https:// www.ncbi.nlm.nih.gov/ books/ NBK559266/
2) Ali HA, Lippmann M, Mundathaje U, Khaleeq G. Spontaneous hemothorax: a comprehensive review. Chest 2008; 134: 1056-65.
3) Prado-Calleros HM, Jiménez-Fuentes E, Jiménez-Escobar I. Descending necrotizing mediastinitis: systematic review on its treatment in the last 6 years, 75 years after its description. Head Neck 2016; 38: E2275-E83.



