

Summary
Background: Some of the residual effusion cannot be drained by the chest tube due to the high port position of the uniportal video-assisted thoracoscopic surgery (VATS) which theoretically leads to prolonged hospital stay. Hypothesis that putting an additional small catheter drain at the most depended part of the hemi-thorax together with chest tube after uniportal VATS to evaluate value of small catheter drainage with chest tube after uniportal VATS in hospital stay, pain score and chest x-ray.Materials and Methods: It represents a pilot prospective study randomized trial from August 2019 to August 2020 who had undergone uniportal VATS procedures were divided into two groups as group A (chest tube with small catheter) and group B (chest tube only).
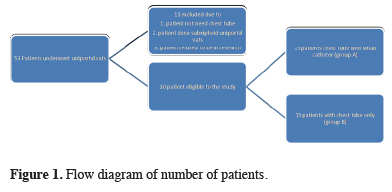
Results: Fifty-three patients underwent uniportal VATS only 30 where eligible to the study divided into two equal groups (18 males, 12 females). The mean age of patients in the small catheter with chest tube was 42.07 ± 12.85 years, compared to 34.93 ± 10.73 years in the chest tube only. Six different types of operation was done. Postoperative pain and hospital stays was nearly equal in both groups (p > 0.05). Postoperative residual effusion in immediate chest x-ray in small catheter with chest tube was managed by aspiration from small catheter and show improvement in follow up chest x-ray next morning (p < 0.05) but in chest tube only was management conservatively didn’t show improvement in follow up chest x-ray next morning (p > 0.05).
Conclusions: Small catheter with chest tube didn’t add more pain. Although more than half of the cases get aspiration from small catheter and show improvement in follow up chest x-ray next morning, this does not statically affect hospital stay.
Introduction
Video-assisted thoracoscopic surgery (VATS) is now considered a minimally invasive technique among thoracic surgeons. VATS surgeons attributed the origin of thoracoscopic therapy to the Swedish physician Hans Christian Jacobaeus 1912 [1]. VATS causes less pain, postoperative complications and shortened hospital stay due to the decreased trauma to the chest wall. It has become superior to many diagnostic and therapeutic procedures that require traditional thoracotomy [2,3]. Thoracotomy is considered as one of the most painful surgical procedures. Increase postoperative pain lead to complications such as retained secretion, limited physical activity, atelectasis and pneumonia [4]. Most of the progress in these areas was accomplished by Gaetano Rocco’s group at the National Cancer Institute, Italy. In June 2010, a significant milestone in this approach occurred with the world’s first uniportal VATS lobectomy, which was reported in 2011 by Gonzalez Rivas’s group in Coruna, Spain. Ever since, uniportal VATS has been successfully used to perform complex lung resection procedures involving pneumonectomy, segmentectomy, bronchoplastic and chest wall resection. There are promising initial clinical outcomes and short term results, and further data is awaited in the long run [5,6]. Recent systematic reviews report that VATS increases survival in early-stage lung cancer [7].An intercostal tube is applied intra-operative following traditional VATS procedures to drain the remaining pneumothorax and residual effusion, traditionally via two chest tubes, one to air drainage directed up and another for fluid drainage directed downward. In uniportal VATS, surgeons almost always put one chest tube with subsequent outstanding possibility of ineffective drainage due to the high position of the chest tube at 5th and sometimes 4th intercostal space [8]. If no suction is applied, some of the residual effusion can’t drain through the intercostal tube, resulting in a prolonged hospital stay.
The hypothesis is that placing additional small catheter drainage at the most depended part of the hemi-thorax in conjunction with the chest tube can result in the chest tube being removed earlier without causing the additional patient pain, hospital stay, or additional incision for another chest tube .
Methods
This work was conducted in Cardiothoracic Surgery Department of Assiut University Heart Hospital. It is a pilot prospective study randomized trial (coin tossing) in which patients admitted to the service between August 2019 and August 2020 who underwent uniportal VATS procedures. Fifty-three patients underwent uniportal VATS only 30 where eligible to the study were divided into two equal groups as group A: chest tube with small catheter drainage and group B: chest tube only (Figure 1).
 Click Here to Zoom |
Figure 1: Flow diagram of number of patients. |
The inclusion criteria for the study are; patients who underwent uniportal video-assisted thoracoscopic surgery at our hospital and require postoperative chest drainage. The exclusion criteria are; patients who did not require the insertion of an intercostal tube post-operatively and refused to be in research. Perioperative management is achieved by the same team of surgeons who performed all the operations that was decortication, lung resection (lobectomy or sublobar resection), drainage and sympathectomy nearly same on both groups. The incision was created in the fourth or fifth intercostal space between the anterior axillary line and the midaxillary line. The chest tube was inserted into the fourth or fifth anterior axillary line and placed anteriorly to the apex of the chest, and the chest tube was connected to water sealed bottles. A guide-wire was used to guide the insertion of a small-bore drain. Central veins catheter was used as small catheter drainage, we use 4, 5, or 7 Fr size depending on the patient’s weight and age. A needle and syringe were used to localize the insertion position for the video thoracoscope [9]. After passing a guide-wire through the needle’s hub, the needle was removed and the tract was enlarged with a dilator. A small-bore tube can then be passed into the thoracic cavity along the wire (Figure 2).
 Click Here to Zoom |
Figure 2: Small catheter drainage in the most dependent part. |
Operative time from the skin incision to skin closure was calculated by min. The severity of pain was quantified using numerical rating scales. The score ranged from zero to 10; no pain results in a zero on the numerical rating scale (NRS), whereas severe pain results in a ten on the NRS. Hospital stays mean from the day of surgery to the day of discharge. After removing the chest tube; the chest drains less than 50 mL per day with no air leak and minimal osculation. Small catheter should be removed following chest tube removal if the lung is fully expanded and there is no residual effusion in chest x-ray and aspiration from the small catheter is less than 10 mL and aspiration done by using syringe 50 mL. Chest x-rays was performed at 4 hour post-operatively and following morning. Complications were based on postoperative persistence air leak, subcutaneous surgical emphysema, bleeding and wound infection. Ethical consideration is based on risk/benefit assessment. The data gathered in this study may aid in increasing the number of patients undergoing VATS, including those who participate in this study. On the other hand, patients would benefit from the clinical and radiological follow-up. Patients undergoing VATS would benefit from significant impact of early postoperative discharge, resulting in reducing pain and lowering morbidity and mortality percentage. There are no known risks associated with participation in this study except for risk of exposure to anesthesia in the operative procedures. No alteration will be made the patients’ treatment or follow-up. Dealing with data and data dissemination should be confidential. The investigators reviewed the charts to determine patients’ eligibility, and collect necessary variables in a private area at the cardiothoracic department to ensure confidentiality. The data from the eligible charts were kept in locked cabinets. Each patient was assigned a specific study number, which was used to enter the data into the computers for analysis and statistical purposes. The computers were password protected, and no one except the investigators would have access to the cabinets, study coding numbers or computers. Identifiable data were accessed only by the investigators and were not shared with any other doctors. An informed written consent will be obtained from those patients who will participate in the study mentioning the risk of the procedure and associated anesthesia. We ask also the consent as if they will undergo any specific intervention and their management will be the usual management of patient with VATS. A small catheter drainage with chest tube after VATS not done before and we will inform the patient about this.
The committee of medical ethics of faculty of medicine approved our research (No: 17100559).
Statistical Analysis
The data were tested for normality using the Kolmogorov-Smirnov test and for homogeneity variances prior to further statistical analysis. Categorical variables were described by number and percent, where continuous variables described by mean and standard deviation. Differences between the groups for categorical variables were analyzed using Chi Square test or Fisher’s Exact test. Student’s t test was used to assess difference between two groups in terms of and continuous variables. A two-tailed p < 0.05 was considered statistically significant. All analyses were performed with the IBM SPSS 20.0 software.
Results
Fifty-three patients underwent uniportal VATS only 30 where eligible to the study divided into two equal groups (18 males, 12 females). The mean age of patients in the small catheter with chest tube was 42.07 ± 12.85 years, compared to 34.93 ± 10.73 years in the chest tube only. The small catheter with chest tube showed a male dominance by 66.7%, while chest tube only had a nearly equal distribution regarding the male to female ratio (Table 1).Table 1: Demographic data of patient in both groups.
Six different type of operation includes decortication, lung resection (lobectomy or sublobar resection), drainage and sympathectomy nearly same on both groups (p > 0.05).
Post-operative pain mean score immediately following operation: the small catheter with chest tube scored 4.46 ± 1.27 while the chest tube only 4.79 ± 0.58. The mean pain score for the 6-hour in small catheter with chest tube was 3.46 ± 1.33 while chest tube only had a mean 3.86 ± 0.77. Pain score next morning small catheter with chest tube has a mean 3 ± 1.58, while the chest tube only mean was 3.21 ± 0.7. Mean duration of air leak in the small catheter with chest tube was 2.01 ± 1.94 days, while in the chest tube only was 2.33 ± 2.42 days. Mean duration of chest tube in the small catheter with chest tube was 4.58 ± 3.75 days, while in the chest tube only was 2.93 ± 2.79 days. The number of patients in the small catheter with chest tube who had a postoperative pneumothorax on an immediate chest x-ray was 7 (46%); the number of patients in the small catheter with chest tube who had a next morning pneumothorax on a chest x-ray in small catheter with chest tube was 4 (26%). In chest tube only postoperative pneumothorax in immediate chest x-ray was 4(26%) next morning pneumothorax in chest x-ray was 3(20%). No significant difference between two groups in duration of air leak (p > 0.05).
The number of patients in the small catheter with chest tube that showed postoperative residual effusion in immediate chest x-ray in the small catheter with chest tube was 10 patients, all of which were managed by aspiration from small catheter. The following day residual effusion in chest x-ray in the small catheter with chest tube was 4 patients (p = 0.028). In the chest tube only postoperative residual effusion in immediate chest x-ray was 3 patients next morning residual effusion in chest x-ray is the same 3 patients (p = 1.000).
There was no need for another chest tube during period of admission in both groups. There was no additional complication such as wound infection and chest infection reported in either groups. Only one case required surgical emphysema management conservative (p = 0.309).
Small catheter with chest tube patients stayed a mean of 4.38 ± 1.8 days in the hospital following surgery, while those in the chest tube only spent a mean of 3.33 ± 2.77 days (p > 0.05).
There were no statically difference between two groups regarding: pain score, hospital stay or post-operative complications; However there was statically difference regarding post-operative pleural effusion, small catheter with chest tube was superior in management of post-operative pleural effusion (p = 0.028) in comparison to chest tube only which showed no statically significant in management of pleural effusion (p = 1.000).
Follow-up chest x-rays performed ten days after patient were discharged revealed no difference between two groups. There were four patients in the study and group B, two patients in each group, had an obliteration of the costophrenic angle on chest x-rays.
Discussion
The study set out to investigate the significance of small catheter drainage with chest tube protocol in patients undergoing VATS surgery vs. Chest tube only, by comparing the patients’ postoperative pain grade, hospital stay, and postoperative chest x-rays as well as their need for re-insertion of an intercostal tube or any additional management.Video-assisted thoracoscopic surgery is a diagnostic and therapeutic tool used in the management of pleural, parenchyma, and mediastinal diseases [10]. The small catheter drain is inserted easily, and the procedure is painless if it performed alone for effusion drainage. However, using the small catheter alone may have adverse consequences as severe subcutaneous emphysema and might become blocked by blood clots which is a risk factor, mainly if postoperative bleeding occurs [11].
Yang Z et al concluded that attaching a pigtail catheter to the chest drain through a single incision VATS lobectomy appears to be a safe and promising technique for reducing pain, decreasing air leak time, shortening hospital stay and detecting postoperative bleeding early [12].
It has been demonstrated that patients in the pigtail tube group had a significant more volume drained in a short amount of time on the first 2 days than those in the larger drain group. There were no significant differences between the two groups in the air leak time, subcutaneous emphysema or wound healing same as demonstrated in the present study[12].
In our study, post discharge pleural effusion occurred in two patients in the group A and two patients in the group B who developed an obliteration of the costophrenic angle on follow-up chest x-ray 10 days after discharge. All patients were managed conservatively without the need to insert another chest tube. According to Yang et al report, the percentage of patients that developed pleural effusion after two weeks was two patients in the smaller pigtail group and eleven patients in the larger drain group [12]. All patients were managed conservatively except three in the larger drain group who required chest tube re-insertion.
The pigtail used as small catheter in the Yang Z study had a diameter of 8 Fr [12]. We used central vein catheter as small catheter drainage 4, 5, 7 Fr in size in our study.
Our study’s overall mean length of stay was 4.3 days in the group A and 3.3 days in the group B, which was nearly identical in both groups. Yang et al found that the mean hospital stays was 5 days in pigtail group and 6 days in large drain group [12]. This difference was because of some of minor procedure in our study, such as uniportal VATS biopsy, were performed as a one-day procedure and early discharge from the hospital was the standard. Ismail et al [13]. Reported an average hospital stay of 8.3 days, which differs from our study because Ismail reported a major uniportal VATS operation that requires post-operative physiotherapy and management to fully expand the lung, not to mention the fact that his series’ mean age was also higher than ours.
In our study, the main post-operative pain score was 3 in the group A and 3.3 in the group B on the second day, which was nearly identical in both groups. Yang el al found that pain scores were 3 in the pigtail group and 3 in the large drain group on the second day. These results are consistent with our study, which found no difference in pain scores on the second day, but Yang’s report found that the smaller pigtail group’s pain score decreased significantly on the third day following surgery compared to the larger drain group (p < 0.001).
There is no significant difference between the two groups in terms of sex and age. Small catheters with chest tubes did not add more pain to the patient compared to the chest tube only.
The group A had ten patients (67%) with post-operative residual effusion on immediate chest x-ray, all of whom were managed with aspiration from a small catheter. The following morning, the group A had a residual effusion on chest x-ray was 4 (27%). In the group B, post-operative residual effusion in the immediate chest x-ray was 3 (20%) and in the following day, residual effusion in the chest x-ray was the same 3 (20%) with p-values of 0.028 and 1.000 in the study and group B, respectively. Although some cases were aspirated from a small catheter and showed improvement on the following morning’s chest x-ray, this had no effect on the length of hospital stay for the two groups.
There was no need for another chest tube during the admission period in either the small catheter with chest tube or the chest tube only, except for one case that required conservative surgical emphysema management. The length of stay in the hospital following surgery is nearly identical in both groups.
Limitations of the study
Our study had a limited number of patients, which can be attributed back to the decreased number of cases presented to our center that matched the criteria of the study during the time of the study. Although our study managed to involve many varieties regarding VATS procedures the number of patients in each category didn’t allow for separate comparison of each of the different categories. Lack of publication in the English literature regarding the topic of the study didn’t allow the possibility of comparing our results.
In conclusion a small catheter with a chest tube did not add more pain to the patient comparing to a chest tube only. Although more than half of the cases get aspiration from the small catheter and show improvement in follow-up chest x-ray the following day, this does not statically affect hospital stay.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics approval
The study was approved by the Ethics Committee of Assiut University, Faculty of Medicine, Egypt (RIBno: 17100559).
Authors’ contribution
AA; Data collection, HE; analysis of data, performing surgery, MO; revising the manuscript, AE; writing the overall manuscript. All authors have read and approved the manuscript.
Reference
1) Sihoe AD. The Evolution of VATS Lobectomy, Topics in Thoracic Surgery, Prof. Paulo Cardoso (Ed.), InTech, Available from: http://www.intechopen.com/books/topics-in-thoracicsurgery/the-evolution-of-vats-lobectomy.
2) El-Badry MM, Elkhayat H, Makhlouf GA, Ghoneim A. Intra-operative removal of chest tube in video-assisted thoracoscopic procedures. J Egypt Soc Cardiothorac Surg 2017; 25: 362-8.
3) Elkhayat H, Rivas DG. Long-term survival following thoracoscopic versus open lobectomy for stage I non-small cell lung cancer. Ann Transl Med 2019; 7: S147.
4) Cansever L, Sezen CB, Bedirhan MA. Evaluation of the effect of video-assisted thoracoscopic surgery on early postoperative pain and quality of life. Curr Thorac Surg 2019; 4: 114-9.
5) Ng CS, Lau KK, Gonzalez-Rivas D, Rocco G. Evolution in surgical approach and techniques for lung cancer. Thorax 2013; 68: 681.
6) Ng CS. Uniportal VATS in Asia. J Thorac Dis 2013; 5: S221-5.
7) Sezen CB, Kocatürk Cİ. Videothoracoscopic lobectomy training in non-small cell lung cancer. Turk Gogus Kalp Damar Cerrahisi Derg 2019; 27: 199-205.
8) Son BS, Park JM, Seok JP, Kim DH. Modified incision and closure techniques for single-incision thoracoscopic lobectomy. Ann Thorac Surg 2015; 99: 349-51.
9) Laws D, Neville E, Duffy J. Pleural Diseases Group, Standards of Care Committee, British Thoracic Society. BTS guidelines for the insertion of a chest drain. Thorax 2003; 58: ii53-9.
10) Kocatürk C, Kutluk AC, Usluer O, Onat S, Çınar HU, Yanık F et al. Comparison of awake and intubated video-assisted thoracoscopic surgery in the diagnosis of pleural diseases: A prospective multicenter randomized trial. Turk Gogus Kalp Damar Cerrahisi Derg 2019; 27: 550-6.
11) Kejriwal NK, Newman MA. Use of a single silastic chest drain following thoracotomy: initial evaluation. ANZ J Surg 2005; 75: 710-2.



