

Summary
Background: Thoracic computed tomography (CT) scans for preliminary diagnosis of COVID-19 can be used as a tool to detect solitary pulmonary nodules (SPNs).Materials and Methods: We retrospectively evaluated the thoracic CT reports of 5416 patients, aged 45-75, who presented to our hospital with a preliminary diagnosis of COVID-19 in 2020.
Results: Pulmonary nodules/masses were detected in 85 patients. 56 of these were male, and 29 female. 63 patients (74%) had SPNs, 11 (13%) masses, and 11 (13%) multiple nodules. 5 patients were in follow-up for malignancy, and 21 (21%) arrived for follow-up after the detection of nodule/mass. 11 patients died due to pulmonary pathologies.
Conclusions: COVID-19-related concerns have seriously disrupted the follow-up of pulmonary nodules. However, the widespread use of CT serves as a kind of lung cancer screening.
Introduction
The SARS-CoV-2 epidemic, which started in China’s Wuhan province at the end of 2019, spread worldwide and was declared a pandemic by the World Health Organization, affecting all countries and causing thousands of deaths and hospitalizations every day [1].The most common clinical presentation in COVID-19 is respiratory distress, and as in other viral diseases, pulmonary involvement manifests as ground-glass opacity (GGO), rendering chest x-ray insufficient. Therefore, computed tomography (CT) has become standard in COVID-19 diagnosis [2].
During the pandemic, frequent thoracic CT scans have almost proved to be a screening program for detecting parenchymal nodules and masses since lung cancer requires early treatment for favorable outcomes but usually progresses asymptomatically in the early stage and is detected incidentally [3-5].
In the present study, we reassessed the thoracic CT scans taken for preliminary diagnosis of COVID-19 in our clinic and investigated the cases with solitary pulmonary nodules (SPNs) and masses.
Methods
We evaluated patients aged 45-75 with thoracic CT scans taken for preliminary diagnosis of COVID-19 in our hospital, between March and December 2020. We retrospectively assessed their thoracic CT reports to detect non-COVID-19 findings.Our hospital database enabled us to refer to both the previous and later scans of the patients with non-COVID-19 findings. We included patients with pulmonary nodule on the CT reports and nodule sized > 5 mm and excluded extraparenchymal pathologies. Besides, nodules < 5 mm in size remained outside our investigation since they required no further evaluation [6].
We retrospectively evaluated the patients’ age, gender, tumor size and location, previous and later CT findings, history of malignancy, and survival.
Ministry of Health and local ethics committee of Omer Halisdemir University approved the study. Informed consent was taken from all participants.
Results
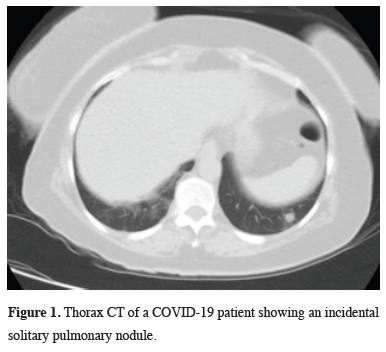
We evaluated the CT reports of 5416 patients conforming to the inclusion criteria. It was observed that all patients had low-dose CT and the reporting was mixed by 4 separate radiologists working in our hospital and from a private center through external reporting.Intraparenchymal nodule (>5 mm) or mass was detected in 85 patients (0.15%). The mean size of SPNs was 21.7 mm, and masses 49.1 mm (Figures 1,2).
 Click Here to Zoom |
Figure 1: Thorax CT of a COVID-19 patient showing an incidental solitary pulmonary nodule. |
 Click Here to Zoom |
Figure 2: Thorax CT of a COVID-19 suspected patient showing a semisolid nodule. |
General characteristics of the patients and information about the nodule are given in table 1. Three 3 patients had a history of lung malignancy, 1 breast, and 1 rectal malignancy, and all were in follow-up. Twenty one (24%) patients had previous CT scans for other reasons, and 18 (21%) had a control CT scan following the detection of a lesion.
It was determined that 11 patients (%13) died during the research. Since patients with a diagnosis of metastatic disease also had additional comorbidities like history of coronary artery disease and the causes of death were not clear, a clear interpretation of death due to the disease could not be made.
Discussion
The COVID-19 pandemic established the routine of thoracic CT scans to assess viral pneumonia findings [2]. In this regard, the number of thoracic CT scans (n = 5416) performed in our center last year for a preliminary diagnosis of COVID-19 only in patients aged 45-75 is remarkable by itself. However, these procedures, along with the regular ones, burdened radiology units with an enormous reporting workload, inevitably prompting efforts at standardization and the development of assessment tools, such as the COVID-19 Reporting and Data System (CO-RADS) [7].Although we evaluated the age range of 45-75 years in our study, patients aged 55-74 years and with a smoking history of more than 30 packs/year are considered high-risk in the NCCN guideline, while patients under the age of 50 and with a smoking history of less than 20 packs/year are considered low-risk [8]. Since we included patients who were evaluated in the emergency room and during the diagnosis of COVID-19, we could not reach the smoking history retrospectively, therefore, we determined the upper limit as 75 years old in accordance with the guideline, while the lower limit was 45 years old. However, since this study aims to screen for pulmonary nodules and lung cancer in the general population of the population only through a specific sample, different evaluations that will be made independent of the age factor will also contribute to the literature.
At our center, we constantly review the effectiveness of CO-RADS and similar classification systems in the prognosis and decision process. However, all this endeavor concerning COVID-19 causes additional pathologies in thoracic CT scans to be overlooked during evaluations. This fact also constitutes a primary limitation in our study since we conducted our investigation based on CT reports retrospectively, not confirming additional pathologies. Nevertheless, reports inconsistent with tomographic images are not rare in clinical practice. A general literature review, coupled with the knowledge that a previous study had indicated the incidental pulmonary nodule frequency in Turkey as 21.8% for patients aged > 55 and nodules > 6 mm, implies that solely evaluating pulmonary involvement COVID-19 can be a limiting factor in detecting incidental nodules [9]. In addition, nodule rates were found to be 10-20% in studies conducted on CT report reading programs in 2014 and 2017 [10]. In another study, the rate of new nodules was observed to be 10% in the evaluation made in the follow-up of patients with cancer [11].
Another limitation is the patients’ reluctance to observe the recommended follow-up program for nodules detected on their initial CT scans because of the COVİD pandemic [12]. Most of our patients (n = 52) did not re-present to our hospital for follow-up, probably due to COVID-19-related fears. In addition, since there was no PET/CT and thoracic surgeon in our hospital at the time period for which the study is planned, it was possible for patients to apply to an external center and these data could not be accessed, so there is no data on the cases followed up in a further center. For this reason, although our study has value in terms of instant nodule detection, more efficient results can be obtained by conducting it in a center where all follow-ups are planned in terms of follow-up strategy and results. This study should be seen as a milestone at this point. According to the Fleischner 2017 guideline for solitary pulmonary nodules, while routine follow-up is not recommended for nodules smaller than 6 mm, 6-12 months follow-up for 6-8 mm, CT or PET/CT and biopsy is recommended 3 months later for solid nodules larger than 8 mm. Routine follow-up is not recommended for subsolid and GGO nodules with sizes smaller than 6 mm too, and for subsolid nodules larger than 6 mm, 3-6 month CT controls are required, and for GGO nodules 3 to 5 years follow-up at 6-12 month interval [13]. Nodule follow-up and advanced imaging and diagnostic procedures to be performed under necessary conditions will increase the diagnosis of early-stage lung cancer [14].
The current literature mainly covers the common challenges and proposed solutions in pulmonary nodule screening during the COVID-19 pandemic and comprehends various cases thought to be nodules at first but later diagnosed with COVID-19 [15,16]. However, to our best knowledge, the present study is the first to evaluate thoracic CT scans taken for COVID-19 preliminary diagnosis in terms of additional pathologies.
Our study focused on the value of CT as a lung cancer screening program rather than the malignancy rates and clinical outcomes of the findings. Lung cancers typically have high survival rates and favorable surgical outcomes if diagnosed early. Early-stage lesions, particularly SPNs, do not cause clinical manifestations in the patient and are usually detected incidentally [17]. This fact increases the diagnostic value of thoracic CTs taken for other reasons [18].
In conclusion, the COVID-19 pandemic has significantly disrupted nodule screening. However, retrospective reassessment of scans and reports may potentially restore the effectiveness of pulmonary nodule screening programs. Any potential the pandemic presents for early diagnosis of lung cancer should be utilized. Our study also emphasized the importance of a holistic evaluation of imaging. Scrutinizing the thoracic CT scans taken for COVID-19 independent of their accompanying reports will offer benefits in detecting additional pathologies. We plan and suggest further studies to support this proposition.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics approval
The study was approved by the institutional review board of Omer Halisdemir University, Faculty of Medicine (No: E-95860085_050.02.04-123708).
Authors’ contribution
MÇ; conceptualized and designed the study, HT; collected and analyzed data. MÇ,HT; revised the final version of the manuscript and co-wrote the paper. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Reference
1) Mohamadian M, Chiti H, Shoghli A, Biglari S, Parsamanesh N, Esmaeilzadeh A. COVID-19: Virology, biology and novel laboratory diagnosis. J Gene Med 2021; 23: e3303.
2) Zheng Q, Lu Y, Lure F, Jaeger S, Lu P. Clinical and radiological features of novel coronavirus pneumonia. J Xray Sci Technol 2020; 28: 391-404.
3) Hirsch FR, Scagliotti GV, Mulshine JL, Kwon R, Curran WJ Jr, Wu YL et al. Lung cancer: current therapies and new targeted treatments. Lancet 2017; 389: 299-311.
4) Wilson R, Devaraj A. Radiomics of pulmonary nodules and lung cancer. Transl Lung Cancer Res 2017; 6: 86-91.
5) Simon M, Zukotynski K, Naeger DM. Pulmonary nodules as incidental findings. CMAJ. 2018 Feb 12;190(6):E167.Nasim F, Ost DE. Management of the solitary pulmonary nodule. Curr Opin Pulm Med 2019; 25: 344-53.
6) Prokop M, van Everdingen W, van Rees Vellinga T, Quarles van Ufford H, Stöger L, Beenen L et al. COVID-19 Standardized Reporting Working Group of the Dutch Radiological Society. CO-RADS: A Categorical CT Assessment Scheme for Patients Suspected of Having COVID-19 -Definition and Evaluation. Radiology 2020; 296: E97-E104.
7) Ettinger DS, Wood DE. Aisner DL, Akerley W, Bauman JR, Bharat A et al. NCCN Guidelines Insights: Non-Small Cell Lung Cancer, Version 2. 2021. Journal of the National Comprehensive Cancer Network: JNCCN 2021; 19: 254–266.
8) Ogan N, Baha A, Özan Sanhal E, Alhan A, Gülhan M. Incidental pulmonary nodule frequency in Turkey. Tuberk Toraks 2019; 67: 190-6.
9) Kang SK, Garry K, Chung R, Moore WH, Iturrate E, Swartz JL et al. Natural Language Processing for Identification of Incidental Pulmonary Nodules in Radiology Reports. J Am Col Radiol 2019; 16: 1587-94.
10) Walter JE, Heuvelmans MA, Yousaf-Khan U, Dorrius MD, Thunnissen E, Schermann A et al. New Subsolid Pulmonary Nodules in Lung Cancer Screening: The NELSON Trial. J Thorac Oncol 2018; 13: 1410-4.
11) Van Haren RM, Delman AM, Turner KM, Waits B, Hemingway M, Shah SA et al. Impact of the COVID-19 Pandemic on Lung Cancer Screening Program and Subsequent Lung Cancer. J Am Coll Surg 2021; 232: 600-5.
12) MacMahon, H, Naidich DP, Goo JM, Lee KS, Leung A, Mayo JR et al. Guidelines for Management of Incidental Pulmonary Nodules Detected on CT Images: From the Fleischner Society. Radiology 2017; 284: 228-43.
13) Cruickshank A, Stieler G, Ameer F. Evaluation of the solitary pulmonary nodule. Intern Med J 2019; 49: 306-15.
14) Varona Porres D, Simó M, Sánchez AL, Cabanzo L, Andreu J. Single pulmonary nodule with reverse halo sign in COVID-19 infection: Incidental finding on FDG PET/CT scan. Med Clin (Barc) 2021; 156: 102.
15) Silva M, Ledda RE, Schiebler M, Balbi M, Sironi S, Milone F et al. Frequency and characterization of ancillary chest CT findings in COVID-19 pneumonia. Br J Radiol 2021; 94: 20200716.



