

Summary
Background: The management of minimal pneumothorax, which has been detected more frequently with the increasing use of computed tomography, especially after blunt trauma, is controversial. This study aimed to examine the results of patients with pneumothorax secondary to blunt trauma and contribute to the treatment protocol for this group of patients.Materials and Methods: A retrospective analysis of patients with pneumothorax after blunt trauma (n = 103) presenting to the emergency department during the 1-year period from January 2019 to January 2020 was performed. Oxygen inhalation was performed in patients who were followed up conservatively, and tube thoracostomy was performed in patients who were treated invasively.
Results: Among 766 patients with blunt trauma, 141 (18.4%) patients had a traumatic pneumothorax. Mechanical ventilation was required in 26.2% (n = 27) patients. Further, 73 (70.8%) patients with pneumothorax were followed up conservatively. The remaining 30 (29.1%) patients underwent tube thoracostomy. The median size of the pneumothorax (9 vs. 29 mm; p < 0.0001; hazard ratio [HR] = 5.08) was significantly different between the groups. Multivariate analyses revealed that positive pressure ventilation and pneumothorax size did not pose an additional risk of failure in conservative management (HR = 1.49; p = 0.25 and HR = 10.2; p = 0.09, respectively). Multivariate analyses revealed that the presence of hemothorax and subcutaneous emphysema (HR = 14.4; p = 0.018 and HR = 13.1; p = 0.019, respectively) led to failure of conservative treatment.
Conclusions: The presence of hemothorax and subcutaneous emphysema was an independent factor leading to failure of conservative treatment. In the presence of these two findings indicating major trauma, invasive treatment is recommended.
Introduction
Thoracic trauma occurs in approximately two-thirds of multiple trauma cases and is the primary cause of mortality in 25% patients with trauma [1]. Traumatic pneumothorax occurs in one-fifth of patients with multiple traumas [2] and is the most significant potentially life-threatening pathology in blunt thoracic trauma [3].In such cases, the ideal treatment method is tube thoracostomy. The management of minimal pneumothorax that cannot be detected by x-rays, which has been detected more frequently with the increasing use of computed tomography (CT), especially after blunt trauma, is controversial.
Tube thoracostomy is not an uncomplicated procedure. A meta-analysis has reported an average complication rate of 19% [4]. In such cases, it is clinically difficult to perform conservative treatment up to the stage at which an invasive procedure should be performed. Although uncomplicated traumatic pneumothorax can be well-tolerated, conservative aproach recommended because tube thoracostomy placement can potentially prevent morbidity and mortality [5].
In the guidelines published by the American College of Surgeons, chest tube insertion is recommended for any traumatic pneumothorax. However, asymptomatic pneumothorax can be managed by observation and aspiration at the discretion of the treating physician. In addition, the need for a chest drain has been reported in patients receiving either general anesthesia or positive pressure ventilation (PPV) to avoid life-threatening pneumothorax [6].
These guidelines are based on the results of cases of large-volume pneumothorax detected by X-ray. Currently, CT scanning is available in almost every trauma unit for patients with multiple traumas, and the frequency of pneumothorax diagnosis at the sub-centimeter level has increased.
Although minimal pneumothorax is encountered incidentally in 2% patients, it can be found in 10% patients after blunt thoracic trauma. This raises the question of whether these small “minimal” pneumothoraxes, which account for 76% of all traumatic pneumothorax cases, can be left untreated, especially when PPV is required [7]. Although an early study has shown a high failure rate in conservatively treated patients receiving PPV [8], studies have suggested that minimal pneumothoraxes, including those in patients receiving PPV, can be managed conservatively [5,7,9-11].
Case studies have also suggested that it is possible to treat larger pneumothoraxes through observation [12]. Therefore, this study aimed to examine the results of patients with pneumothorax secondary to blunt trauma and contribute to the treatment protocol for this group of patients.
Methods
This single-center, retrospective study was conducted at University of Health Sciences, Bakırköy Dr. Sadi Konuk Training and Research Hospital, Department of Thoracic Surgery between January 2019 and January 2020. In addition to demographic information, data on the type of injury, injury severity score, radiological dimension of pneumothorax, additional pathologies, treatment, need for PPV, length of stay (LOS), complications, and mortality were recorded. Oxygen inhalation (2–4 l/min) was performed in patients followed up conservatively, whereas 28–32-F tube was inserted in patients treated with tube thoracostomy. The injury severity score (ISS) was used to determine trauma severity [13]. The ISS is correlated with mortality, morbidity, and hospitalization time after trauma. An ISS of 1–8, 9–15, 16–24, and ≥ 25 indicated minor, moderate, severe, and very severe trauma, respectively [14]. The scoring system described by De-Moya et al. was used to measure the level of pneumothorax observed on thorax CT [15]. The score is composed of two parts; (1) the largest diameter of the air pocket and (2) its relationship with the pulmonary hilum. The first step was to measure the largest air collection along a line perpendicular to the chest wall or mediastinum in millimeters. The pulmonary hilum was then identified, and it was determined whether the pneumothorax crossed the transhilar axial plane. If the pneumothorax line did not cross this plane, 10 was added to the millimeter scale. If the pneumothorax line crossed this plane, 20 was added to the largest dimension measured. The sum of the two numbers was the final score. The study protocol was approved by the University of Health Sciences, Bakırköy Dr. Sadi Konuk Training and Research Hospital Ethics Committee (date/no: 05.04.2021/2021/193).
Statistical Analysis
Non-parametric methods were used to compare the two independent groups because of the small number of patients recruited in the study. Fisher’s exact test was used to compare categorical variables, whereas the Mann–Whitney U test was used to compare continuous or ordinal variables.
Receiver operating characteristic (ROC) analysis was used to successfully estimate the pneumothorax size and De Moya score for optimal cutoff points in conservative follow-up. Univariate analysis was used to compare patients undergoing and not undergoing chest tube insertion after CT. Factors with p < 0.1 were then entered into a backward stepwise likelihood regression model. In the model, statistical significance was set at p ≤ 0.05. Data were analyzed using IBM SPSS Statistics version 20 (IBM Corp., Armonk, NY, USA).
Results
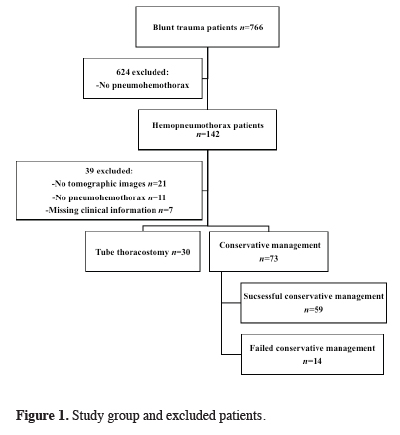
Between January 2019 and January 2020, among 766 patients with blunt trauma who underwent emergency surgery, 142 patients had hemopneumothorax secondary to blunt trauma. After excluding patients who did not meet the study criteria, 103 patients were analyzed (Figure 1).
 Click Here to Zoom |
Figure 1: Study group and excluded patients. |
Table 1 summarizes the demographic characteristics, type of injury, ISS, pneumothorax characteristics, management, and treatment results of the non-conservatively and conservatively managed patients. Among 766 patients with blunt trauma, 141 (18.4%) patients had a traumatic pneumothorax.
The mean age of the patients was 43.5 (standard deviation [SD] = 19.3), and most patients were men (n = 74, 71.8%). The most common type of trauma was falling (n = 46, 44.6%). The mean ISS was calculated as 8.7 (SD =6.5), which was defined as non-major traumas [14]. Mechanical ventilation and intensive care were required in 26.2% (n = 27) patients. In a series of 103 patients, mortality occurred in eight (7.8%) patients.
Table 2 summarizes the characteristics and outcomes of successful and failed observational management.
Table 2: Characteristics and outcomes of conservatively managed patients.
In total, 73 (70.8%) patients with pneumothorax were followed up with conservative methods and observational treatments. The remaining 30 (29.1%) patients underwent tube thoracostomy. Regarding the comparison of the pneumothorax size, patients followed up conservatively had a significantly smaller pneumothorax than those who underwent tube thoracostomy (median, 9 vs. 29 mm; p < 0.0001). This difference was also observed in the De-Moya score (median, 19 vs. 45.5; p < 0.0001).
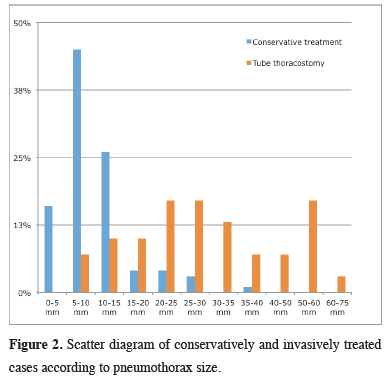
The distribution of patients treated conservatively and invasively according to the pneumothorax size is shown in Figure 2. The pneumothorax size was <10 mm in most patients who were followed up conservatively.
 Click Here to Zoom |
Figure 2: Scatter diagram of conservatively and invasively treated cases according to pneumothorax size. |
The invasively treated group had more severe trauma, a higher ISS (mean 12.4 vs 7.2; p = 0.0002), more frequent need for intensive care (40% vs. 20.5%; p = 0.04), more frequent hemothorax (53.3% vs. 26%; p = 0.008), more frequent lung contusion (83.3% vs. 56.1%; p = 0.009), and more frequent rib fracture (86.6% vs. 61.6%; p = 0.013) than the conservatively treated group.
There were no significant differences between the two groups in terms of age, sex, type of trauma, and length of stay
The mortality rate was higher in the invasively treated group than in the conservatively treated group (20% vs. 2.7%; p = 0.003).
Among 73 patients treated conservatively, 59 (80.8%) patients did not require additional interventions. Mechanical ventilation was performed in 15 (20.3%) patients treated conservatively. Among 14 patients requiring additional intervention, seven (50%) patients were treated with mechanical ventilation, and this rate was significantly higher than that in the successful conservative treatment group (50% vs. 13.5%; p = 0.002).
Based on the univariate analysis results, age, sex, ISS, presence of lung contusion, and rib fracture were not significantly related to failure of conservative treatment (Table 3).
Table 3: Hazard ratios for failed conservative management.
The median pneumothorax size (9 vs. 29 mm; p < 0.0001; hazard ratio [HR] = 5.08) and median De-Moya score (19 vs. 45.5; p < 0.0001; HR = 3.7) were significantly different between the groups.
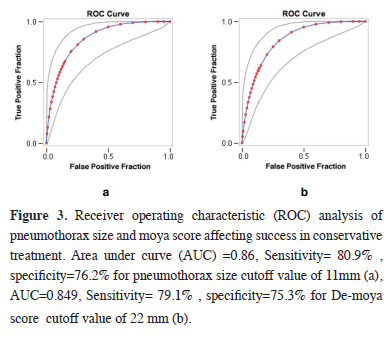
To indicate when to discontinue conservative pneumothorax treatment, the cutoff size of the pneumothorax was determined to be 11 mm using the ROC curve. The optimal cutoff value for the De-Moya scoring system was 22 (Figure 3).
 Click Here to Zoom |
Figure 3: Receiver operating characteristic (ROC) analysis of pneumothorax size and moya score affecting success in conservative treatment. Area under curve (AUC) =0.86, Sensitivity= 80.9% , specificity=76.2% for pneumothorax size cutoff value of 11mm (a), AUC=0.849, Sensitivity= 79.1% , specificity=75.3% for De-moya score cutoff value of 22 mm (b). |
However, when the pneumothorax size data were evaluated using multivariate analysis, its effect on failure of conservative treatment was not found to be statistically significant (Table 4). Multivariate analyses revealed that PPV did not pose an additional risk of failure in conservative management (HR = 1.49; p = 0.25). In contrast, multivariate Cox regression analysis revealed that the presence of hemothorax and subcutaneous emphysema (HR = 14.4; p = 0.018 and HR = 13.1; p = 0.019, respectively) led to failure of conservative treatment (Table 4).
Table 4: Multivariable Cox regression analysis for failure of conservative management.
The mean ISS of the eight patients who died was 26.4 (>25 representing serious or critical injuries). In five of eight cases, the patients died due to cranial traumatic pathologies, and in the remaining three cases, the patients died due to uncontrollable abdominal bleeding (the liver, spleen, and inferior vena cava).
Discussion
Tube thoracostomy is a procedure with a complication risk ranging from 15% to 30% [11,16,17]. The current guidelines recommend chest tube insertion for traumatic pneumothorax, especially in patients receiving ventilation support, even if they are asymptomatic [6]. Asymptomatic patients who do not require a ventilator can be managed by observation or aspiration at the physician’s discretion.Some studies have reported that conservative treatment can be used in selected patients to determine whether minimal pneumothorax can be managed conservatively [5,11].
Studies on scoring systems that determine whether chest tube intervention is necessary for occult pneumothorax and those with larger patient groups are needed [15].
This study aimed to determine whether pneumothorax secondary to blunt trauma could be treated conservatively and examine situations requiring chest tube insertion.
In this study, positive pressure ventilation (PPV) did not pose a risk in terms of conservative treatment.
Studies have been focused on the role of conservative treatment in occult pneumothorax not initially visible on radiography [5,11].
Positive findings, including those in patients receiving PPV, have been included in the clinical guidelines [18]. Although these studies are useful for establishing treatment methods for traumatic pneumothorax, they have limitations.
Currently, CT scanning has become routine in emergency departments, especially for patients with multiple traumas. However, guidelines mainly based on radiographic findings are lacking.
Whether a pneumothorax is visible on radiography not only is related to its size but can also be affected by other factors. For example, supine chest radiography has been shown to reduce the sensitivity [7].
The increase in CT rates causes more limited pneumothorax cases and constitutes a common decision problem in clinical practice. Hence, in this study, we examined the consequences of traumatic pneumothorax. Most patients (71%) were treated conservatively, and most of them (59 of 73 [81%]) did not require additional intervention.
Among 14 patients requiring additional intervention, seven (50%) patients were treated with mechanical ventilation, and this rate was significantly higher than that in patients successfully treated conservatively (50% vs. 13.5%; p = 0.002). Multivariate analyses revealed that PPV did not pose an additional risk of failure in conservative management (HR =. 1.34; p = 0.21).
This finding is consistent with that the current literature on minimal pneumothorax. Moore et al [11] reported a 14% failure rate when PPV was performed in patients managed via observation. The rate was 4.5% in patients not receiving PPV, but it was identified as an independent predictor of failed management in multivariate analysis. In addition, Brasel et al [10] and Enderson et al [8] reported a high failure rate (22% and 53%, respectively) during conservative follow-up in patients receiving PPV. Although Brasel et al [10] concluded that observation is reliable, Enderson et al [8] recommended tube thoracostomy for all patients requiring PPV. In light of this information, the discussions on the management of occult pneumothorax in patients receiving ventilation support are ongoing. In another study, Hoff et al [19] reported that minimal pneumothorax was observed in stable patients, independent of PPV. The OPTICC trial (ClinicalTrials.gov: NCT00530725) with randomization between chest tube insertion and observation in patients receiving PPV was completed in 2021, and the results are awaited.
Hefny et al found that the need for a tube thoracostomy in pneumothorax secondary to blunt trauma was associated with a pneumothorax volume of more than 30 ml. In this study, pneumothorax volume was calculated using software available in CT [21].
Moore et al. accepted the occult pneumothorax margin as 7mm in their prospective observational study. They found that this cut-off value did not affect success in conservative treatment [11].
Pneumothorax size > 11 mm was found to have a risk of failure in conservative treatment (HR = 5.08; p = 0.01) in univariate analysis. However, when the pneumothorax size data were evaluated in multivariate analysis, the effect on failure of conservative treatment was not found to be statistically significant (HR = 10.2; p =0.09).
Pneumothorax size was previously thought to be a predictor of failure of conservative treatment [20]. To guide treatment, De Moya et al [15] proposed a scoring system that uses the size of occult pneumothorax and its relationship to the hilum. However, Moore et al [11] showed that pneumothorax size was not an independent predictor of failed observations.
Moore et al accepted the occult pneumothorax margin as 7mm in their prospective observational study. They found that this cut-off value did not affect success in conservative treatment[11].
Pneumothorax size is seen as the most important decision-making criterion for tube thoracostomy. However, in cases with minimal pneumothorax secondary to blunt trauma, a decision should be made together with additional pathologies.
In the present study, presence of hemothorax was determined as an independent variable (HR = 14.4; p = 0.018). Walker et al [22] showed that presence of hemothorax was the only independent factor predicting failure of conservative treatment for pneumothorax. This is also considered to be beneficial for patients in clinical practice. Even if draining the blood does not cause a life-threatening problem, it reduces the risk of complications such as infection and fibrothorax in the long term.
In the current study, the presence of subcutaneous emphysema was also found to be an independent variable (HR = 13.1; p = 0.019). Subcutaneous emphysema was interpreted as a sign of a complicated pneumothorax and significant damage to the visceral and parietal pleura. Conservative treatment failure was more common in patients with hemothorax and subcutaneous emphysema. In the presence of these two findings, closer follow-up is required, even if the pneumothorax is small.
Chest ultrasonography is superior to radiography for the diagnosis of pneumothorax in patients with trauma [23,24]. Due to the difficulty of mobilization and close follow-up with x-ray or CT, especially in multi-traumatized cases, it is a candidate to enter ultrasound trauma protocols in which the amount of pneumothorax and hemothorax can be followed together in the management of these cases. Ultrasound may play a useful role in the routine management of thoracic trauma.
The type of injury, ISS, and pneumothorax size were not strong indicators of the need for intervention.
Although the need for ventilation support is controversial, both the current findings and previous study findings [5,11] have shown that pneumothorax can be managed conservatively. Most conservatively treated patients, including those requiring ventilation support and who do not pose an additional risk, were successfully treated without the need for chest drains.
In the presence of a high-volume ventilated lung, tube thoracostomy may be more complicated. Despite the classical guidelines recommending tube thoracostomy for pneumothorax detected in ventilator-dependent patients, the current study suggests that patients with minimal pneumothorax secondary to blunt trauma can be managed conservatively with close monitoring. The presence of hemothorax and subcutaneous emphysema was found to be an independent factor leading to failure of conservative treatment. In the presence of these two findings, indicating major trauma, invasive treatment is recommended.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Ethics approval
Approval for this retrospective, descriptive, single-center study was obtained from the Clinical Research Ethics Committee of Recep Tayyip Erdogan University Faculty of Medicine (decision no: 2020/193, dated 03.09.2020).
Authors’ contribution
Oİ; conceptualized and designed the study, collected and analyzed data, revised the final version of the manuscript and wrote the paper.
Reference
1) Kshettry VR, Bolman RM 3rd. Chest trauma. Assessment, diagnosis, and management. Clin Chest Med 1994; 15: 137-46.
2) Di Bartolomeo S, Sanson G, Nardi G, Scian F, Michelutto V, Lattuada L. A population-based study on pneumothorax in severely traumatized patients. J Trauma 2001; 51: 677-82.
3) Idris BM, Hefny AF. Large pneumothorax in blunt chest trauma: Is a chest drain always necessary in stable patients? A case report. Int J Surg Case Rep 2016; 24: 88-90.
4) Hernandez MC, El Khatib M, Prokop L, Zielinski MD, Aho JM. Complications in tube thoracostomy: Systematic review and meta-analysis. J Trauma Acute Care Surg 2018; 85: 410-6.
5) Wilson H, Ellsmere J, Tallon J, Kirkpatrick A. Occult pneumothorax in the blunt trauma patient: tube thoracostomy or observation? Injury 2009; 40: 928-31.
6) ATLS Subcommittee; American College of Surgeons’ Committee on Trauma; International ATLS working group. Advanced trauma life support (ATLS®): the ninth edition. J Trauma Acute Care Surg 2013; 74: 1363-6.
7) Ball CG, Kirkpatrick AW, Feliciano DV. The occult pneumothorax: what have we learned? Can J Surg 2009; 52: E173-9.
8) Enderson BL, Abdalla R, Frame SB, Casey MT, Gould H, Maull KI. Tube thoracostomy for occult pneumothorax: a prospective randomized study of its use. J Trauma 1993; 35: 726-9; discussion 729-30.
9) Plurad D, Green D, Demetriades D, Rhee P. The increasing use of chest computed tomography for trauma: is it being overutilized? J Trauma 2007; 62: 631-5.
10) Brasel KJ, Stafford RE, Weigelt JA, Tenquist JE, Borgstrom DC. Treatment of occult pneumothoraces from blunt trauma. J Trauma 1999; 46: 987-90; discussion 990-1.
11) Moore FO, Goslar PW, Coimbra R, Velmahos G, Brown CV, Coopwood TB Jr et al. Blunt traumatic occult pneumothorax: is observation safe?-results of a prospective, AAST multicenter study. J Trauma 2011; 70: 1019-23; discussion 1023-5.
12) Brown SGA, Ball EL, Perrin K, Asha SE, Braithwaite I, Egerton-Warburton D, et al; PSP Investigators. Conservative versus Interventional Treatment for Spontaneous Pneumothorax. N Engl J Med 2020; 382: 405-15.
13) Baker SP, O’Neill B, Haddon W, Long WB. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974; 14: 187-96.
14) Copes WS, Champion HR, Sacco WJ, Lawnick MM, Keast SL, Bain LW. The Injury Severity Score revisited. J Trauma 1988; 28: 69-77.
15) de Moya MA, Seaver C, Spaniolas K, Inaba K, Nguyen M, Veltman Y et al. Occult pneumothorax in trauma patients: development of an objective scoring system. J Trauma 2007; 63: 13-7.
16) Etoch SW, Bar-Natan MF, Miller FB, Richardson JD. Tube thoracostomy. Factors related to complications. Arch Surg 1995; 130: 521-5; discussion 525-6.
17) Ball CG, Lord J, Laupland KB, Gmora S, Mulloy RH, Ng AK, Schieman C et al. Chest tube complications: how well are we training our residents? Can J Surg 2007; 50: 450-8
18) Mowery NT, Gunter OL, Collier BR, Diaz JJ Jr, Haut E, Hildreth A, et al. Practice management guidelines for management of hemothorax and occult pneumothorax. J Trauma 2011; 70: 510-8.
19) Hoff WS, Bonadies JA, Cachecho R, Dorlac WC. East Practice Management Guidelines Work Group: update to practice management guidelines for prophylactic antibiotic use in open fractures. J Trauma 2011; 70: 751-4.
20) Garramone RR Jr, Jacobs LM, Sahdev P. An objective method to measure and manage occult pneumothorax. Surg Gynecol Obstet 1991; 173: 257-61.
21) Hefny AF, Kunhivalappil FT, Matev N, Avila NA, Bashir MO, Abu-Zidan FM. Management of computed tomography-detected pneumothorax in patients with blunt trauma: experience from a community-based hospital. Singapore Med J 2018; 59: 150-4.
22) Walker SP, Barratt SL, Thompson J, Maskell NA. Conservative Management in Traumatic Pneumothoraces: An Observational Study. Chest 2018; 153: 946-53.



