

2Thoracic Surgeon, Istanbul, Turkey
3Department of Pulmonology, Selcuk University Medical Faculty, Konya, Turkey DOI : 10.26663/cts.2022.026
Summary
Lung cancer is the most common cause of death due to malignancy and early diagnosis is important for surgical treatment. Endotracheal and endobronchial metastasis after left upper lobectomy is a very rare condition in the patient who was followed up for one year postoperatively. By the presented case, it was aimed to determine the approach and etiology of this clinical condition.Introduction
Non-small cell lung cancer (NSCLC) accounts for approximately 80% of all lung cancers. Early diagnosis is crucial in the effectiveness of surgical treatment [1]. The disease recurrence of primary lung cancer is most common in the first two years after lobectomy [2]. Therefore, frequent postoperative monitoring is required.This case is rare and interesting due to the presence of multiple endobronchial and endotracheal metastases in the first year after lobectomy performed for stage I lung primary squamous cell carcinoma (SCC).
Case Presentation
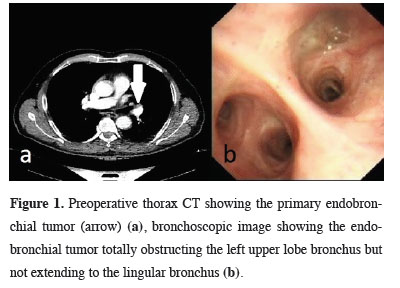
A malignant nodular lesion was detected in the left upper lobe hilum during the examination of a 68-year-old male patient with a presenting complaint of irritant cough. Flexible bronchoscopy revealed a vegetative mass in the left upper lobe bronchus that did not extend to the lingular bronchus (Figure 1).
 Click Here to Zoom |
Figure 1: Preoperative thorax CT showing the primary endobronchial tumor (arrow) (a), bronchoscopic image showing the endobronchial tumor totally obstructing the left upper lobe bronchus but not extending to the lingular bronchus (b). |
After a bronchial biopsy and bronchoalveolar lavage revealed SCC, a left upper lobectomy with thoracotomy was performed after screening for systemic metastasis. The primary lesion was diagnosed as SCC in histopathology and was one cm in diameter, with 34 lymph nodes and bronchial margin biopsies removed during dissection being negative. Definitive diagnosis was stage IA1 lung SCC.
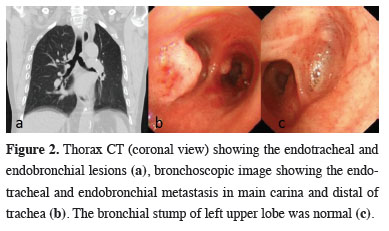
The patient’s follow-up was uneventful until suspicious nodular lesions were detected on the tracheal wall and right main bronchus entrance in the thorax computed tomography taken a year after the surgery, and bronchoscopy was performed again (Figure 2).
 Click Here to Zoom |
Figure 2: Thorax CT (coronal view) showing the endotracheal and endobronchial lesions (a), bronchoscopic image showing the endotracheal and endobronchial metastasis in main carina and distal of trachea (b). The bronchial stump of left upper lobe was normal (c). |
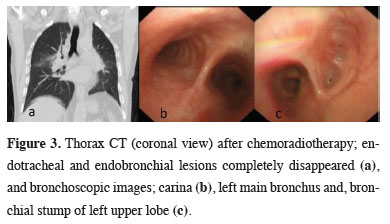
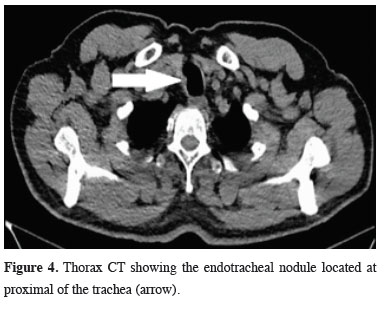
In bronchoscopy, multiple nodular lesions were detected in the posterior and distal trachea, left main bronchus entrance, right main bronchus, and secondary carina. The histopathological results of bronchoalveolar lavage and bronchial biopsy were SCC. PET CT was performed for restaging, and no lesion was detected except for the lesions in the airway. Carboplatin and paclitaxel chemotherapy protocol was applied to the patient and radiotherapy was administered. The lesions completely disappeared after treatment (Figure 3). He received radiotherapy again for the endotracheal lesion that developed in the proximal trachea six months after chemoradiotherapy (Figure 4), and his follow-up continues in the second postoperative year. Written informed consent was obtained from the parents for publication of his data.
 Click Here to Zoom |
Figure 3: Thorax CT (coronal view) after chemoradiotherapy; endotracheal and endobronchial lesions completely disappeared (a), and bronchoscopic images; carina (b), left main bronchus and, bronchial stump of left upper lobe (c). |
 Click Here to Zoom |
Figure 4: Thorax CT showing the endotracheal nodule located at proximal of the trachea (arrow). |
Discussion
Surgery is the most effective treatment for early-stage lung cancer. Particularly, stage I and stage II cases greatly benefit from surgery. Follow-up is continued for intrathoracic or distant organ metastases after surgery. The most common areas of metastasis are the central nervous system, bone, liver, respiratory system, and adrenal glands. Endobronchial and endotracheal metastases of lung cancer are very rare. In the literature, metastasis in the bilateral main bronchus and trachea has rarely been published [3]. During follow-up, the cases may be asymptomatic or may present with respiratory findings such as wheezing and stridor.Recently, the idea of spread through air space (STAS) has come to the fore for lung cancer. Although it is frequently encountered in SCC and adenocarcinoma cases, it has been reported that airway spread is also common in small cell lung carcinoma [4]. It was shown in a study that STAS was encountered in one third of resected lung SCC cases [5]. STAS formation is thought to be related to the spread of loose tumor fragments into the alveolar spaces [6]. Although STAS is encountered in all stages of lung cancer, its frequency increases in metastatic disease and is associated with poor prognosis [6]. Although reasons such as advanced age, sublobar, and limited resection have been suggested, it is known that STAS can be encountered even in complete anatomical resections [5]. In this case, malignant cells were detected in the bronchoalveolar lavage in both bronchoscopies performed before the preoperative diagnosis and after the detection of postoperative metastasis. This result suggests that there may be loose tumor fragments in the primary tumor. Although STAS and endobronchial and endotracheal metastases are conceptually presented as different clinical conditions for lung cancer, there may be a similar cause such as loose tumor fragments in the etiology of both.
In the present case, the detection of endotracheal and endobronchial metastases in the first postoperative year supports these findings in the literature, although left upper lobectomy was performed, and the bronchial margin was negative.
Endobronchial and endotracheal metastases have been associated with poor prognosis. The average surveillance in these cases has been reported as approximately 7.5 months [3]. After the chemoradiotherapy treatment of the presented case was completed, he was followed up for another 6 months without disease and received radiotherapy again due to a new lesion in the proximal trachea.
As in this case, differential diagnosis of STAS or endobronchial metastasis cannot be made on a single case, but we think it would be beneficial to be alert about STAS.
In conclusion, it is necessary to continue frequent follow-ups in operated lung cancer cases, even if they are stage I. Apart from the follow-up of parenchyma and distant organ metastases, it is of great importance that a careful evaluation is made in terms of endobronchial and endotracheal lesions. Endobronchial metastases should be kept in mind by clinicians and radiologists, and they should not avoid bronchoscopy in suspected cases, as small lesions are overlooked on CT. Thus, more studies with large series are needed to demonstrate whether endobronchial or endotracheal metastases are with airway spread. However, patients with malignant preoperative bronchoalveolar lavage should be followed carefully in terms of endobronchial or endotracheal metastases or STAS.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
HY, GSS, FK, AC, HS: conceived and designed the current case report, co-wrote the paper, collected the clinical data. The authors discussed the case under the literature data together and constituted the final manuscript.
Reference
1) Aker C, Sezen CB, Ceritoglu A, Dogru MV, Aksoy Y, Kalafat CE et al. Prognostic value of Glasgow Prognostic Score in patients with non-small cell lung cancers undergoing pN2 pneumonectomy. Curr Thorac Surg 2021; 6: 7-13.
2) Ahuja J, de Groot PM, Shroff GS, Strange CD, Vlahos I, Rajaram R et al. The postoperative chest in lung cancer. Clin Radiol 2022; 77: 6-18.
3) Ito A, Yamaguchi D, Kaneda S, Kawaguchi K, Shimamoto A, Kubooka M et al. Endobronchial brachytherapy as definitive treatment for endobronchial metastasis after surgery of non-small cell lung cancer. World J Surg Oncol 2021; 19: 322.
4) Toyokawa G, Yamada Y, Tagawa T, Kinoshita F, Kozuma Y, Matsubara T et al. High frequency of spread through air spaces in resected small cell lung cancer. Anticancer Res 2018; 38: 1821-5.



