

2Department of Statistics, Faculty of Science, Hacettepe University, Ankara, Turkey DOI : 10.26663/cts.2016.0003
Summary
Background: Tumor size is one of the major prognostic determinants of non-small cell lung cancer (NSCLC). In the present study, we evaluated the effect of tumor size on survival in pN0M0 NSCLC patients.Materials and Methods: Between 1994 and 2013, 1975 NSCLC patients underwent surgery in our center. The study included 774 NSCLC patients with pathological stage N0M0, and these patients were divided into 8 groups according to tumor diameter, as follows, Group 1: 0-10 mm, Group 2: 11-20 mm, Group 3: 21-30 mm, Group 4: 31-40 mm, Group 5: 41-50 mm, Group 6: 51-60 mm, Group 7: 61-70 mm, and Group 8: > 70 mm. We aimed to evaluate the prognostic effect of tumor size on overall survival and to determine a cut-off point for tumor size.
Results: The 5 year overall survival rate for groups 1 to 8 were 85.6%, 81.3%, 68.6%, 62.2%, 55%, 54.2%, 54.3%, and 45.6%, respectively. The mean follow-up time was 43.8 months. In multivariate analysis, age, tumor size, and surgical resection type had an independent prognostic value on survival.
Conclusions: Tumor size is an independent prognostic factor for pN0M0 NSCLC patients. A tumor size of 4 cm was found to be the most suitable cut-off point for survival which may be of help in decision-making for adjuvant chemotherapy.
Introduction
Tumor size is one of the major prognostic determinants of non-small cell lung cancer. In the Eighth edition of the TNM Classification of Lung Cancer, IASLC recommended to sub classify T1 into T1a (≤1 cm), T1b (>1 to ≤2 cm), and T1c (>2 to ≤3 cm); T2 into T2a (>3 to ≤4 cm) and T2b (>4 to ≤5 cm); and reclassify T3 tumors as >5 cm to ≤7 cm and T4 tumors as >7 cm. Tumor size is a well-established prognostic factor. The statistical analysis was performed in a cohort of patients with pN0M0R0, pN0M0Rx, pNxM0R0 and cN0M0 diseases. The T descriptors within the same group were analyzed separately. There is a complex set of analysis and comparisons [1]. The best subset of patients to study the effect of tumor size on survival is pN0M0 group. By using this group, the confounding effect of nodal metastasis is removed. Another important issue is when to give adjuvant therapy in pN0 patients. In this study, we aimed to evaluate the effect of tumor size on survival in NSCLC patients with pathological stage N0M0.Methods
This is a retrospective single center study. Between 1994 and 2013, 1975 non-small cell lung cancer patients underwent surgery in Ankara University School of Medicine Thoracic Surgery Department. We only included pN0M0 NSCLC patients. Patients with lymph node metastases, those without lymph node examination or without appropriate staging information and those with metastasis were excluded. The data of age, sex, tumor diameter, tumor histology, resection type, pathological T stage and overall survival (time between surgery and death) were recorded from the medical files. We declare that the study was performed in accordance with the ethical standards laid down in the Helsinki Declaration of 1975, as revised in 1983. The patients were divided into 8 groups according to tumor diameter, as follows, Group 1: 0-10 mm, Group 2: 11-20 mm, Group 3: 21-30 mm, Group 4: 31-40 mm, Group 5: 41-50 mm, Group 6: 51-60 mm, Group 7: 61-70 mm, and Group 8: >70 mm. We used Kaplan-Meier method with log-rank test for univariate analysis and Cox regression analysis (forward stepwise) for multivariate survival analysis. SPSS version 15.0 was used for statistical analysis. The statistical significance level of P was determined as ≤ 0.05.Results
The analysis included 774 patients (87.2% male) with a mean age of 60.4 years (33-84 years).The distribution of the patients according to tumor size was as follows, Group 1: 24 (3.1%), Group 2: 119 (15.4%), Group 3: 178 (23%), Group 4: 140 (18.1%), Group 5: 110 (14.2%), Group 6: 83 (10.8%), Group 7: 50 (6.4%), and Group 8: 70 (9%) patients. The tumor types of the patients were adenocarcinoma [374 (48.3%)], squamous cell carcinoma [393 (50.78%)] and other cell types [7 (0.9%)]. Of the patients, 522 (67.4%) underwent lobectomy, 162 (20.9%) pneumonectomy and 90 (11.63%) sublobar resection. The characteristics of the patients are summarized in Table 1.
Table 1: Patient characteristics
The 5 year overall survival rate for groups 1 to 8 were 85.6%, 81.3%, 68.6%, 62.2%, 55%, 54.2%, 54.3%, and 45.6%, respectively (Figure 1). Mean follow-up time was 43.8 months and median follow-up time was 43 months. Pairwise comparison between the groups for survival showed that survival was significantly longer in Group 2 than that in Group 3 (P = 0.036); the other pairwise comparisons revealed no significant difference; Group 1 vs. Group 2 (P = 0.853), Group 3 vs. Group 4 (P = 0.206), Group 4 vs. Group 5 (P = 0.088), Group 5 vs. Group 6 (P = 0.698), Group 6 vs. Group 7 (P = 0.387), and Group 7 vs. Group 8 (P = 0.305). In multivariate analysis, age, tumor diameter and resection type were found to be independent prognostic factors. Using Group 1 as reference, hazard ratios showed an increased risk for mortality, significance beginning with Group 5. As seen in Table 2 Group 3 has 1.429 and Group 4 has 2.144 times increased risk for mortality over Group 1 which are found statistically insignificant (P = 0.409, P = 0.079) but Group 5, 6, 7 and 8 have 2.910, 2.841, 2.753, 3.878 times increased risk for mortality over Group 1 and all of them are statistically significant (P = 0.015, P = 0.019, P = 0.027, P = 0.002 respectively). For resection types while pneumonectomy and lobectomy have a smiliar risk for mortality (HR = 1.045, P = 0.781), sublobar resection has 2.711 times increased risk for mortality over lobectomy (P = 0.000). We also classified patients in two groups according to tumor diameter as Group 1: ≤4 cm and Group 2: >4 cm, and found that the survival difference between the two groups was statistically significant (P = 0.000) (Figure 2).
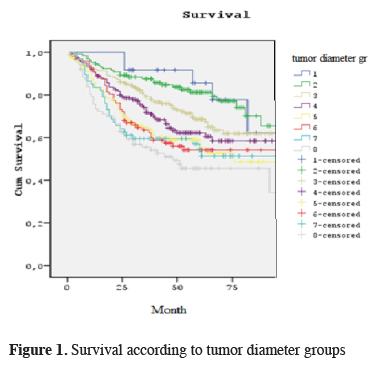
Click Here to ZoomFigure 1: Survival according to tumor diameter groups
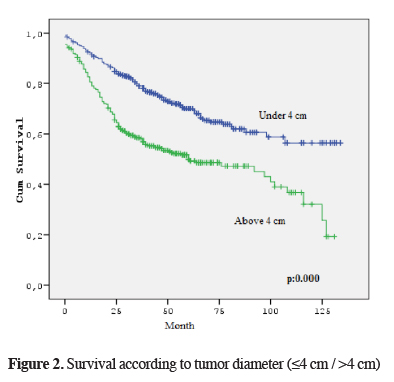
Click Here to ZoomFigure 2: Survival according to tumor diameter (≤4 cm / >4 cm)
Discussion
Tumor size has an important effect on prognosis especially for node negative tumors [2]. In the Eight Edition of IASLC TNM Lung Cancer Staging Project, Rami Porta et al. [1] reported that 5 year survival rates of p N0M0 NSCLC patients with a tumor size 0.1-1 cm, 1.1-2 cm, 2.1-3 cm, 3.1-4 cm, 4.1-5 cm, 5.1-6 cm, 6.1-7 cm were 91%, 86%, 81%, 73%, 66%, 63%, and 58% respectively. Although we found a lower survival rates in the present study, we observed a similar decreasing trend with increasing tumor size.In our study, survival was significantly longer in Group 2 in comparison to that in Group 3 (P = 0.036). This is the 2 cm cut-off point which is used for sublobar resection [3,4]. Our study also showed that sublobar resection has a negative effect on survival compared with lobectomy in multivariate analysis (P = 0.000). These two findings cannot be combined in this study, but it seems that they are important for selecting surgical procedure also for early stage lung cancer.
In multivariate analysis, age, tumor size and surgical resection type have independent prognostic value on survival. When Group 1 was used as reference, we observed that, beginning with group 5 (41-50 mm), hazard ratios showed a significant increasing trend, and also survival difference between the groups with a tumor size ≤4cm and >4 cm was significant, showing that a tumor size of 4 cm seems to be a critical threshold. In the earlier series [5,6] this critical threshold was reported to be 5 cm but in the eight edition of TNM Rami Porta et al. [1] found 3 cm as the most significant cut-off point for T descriptor. Zhang et al. [7] studied similar patient groups and found similar results in multivariate analysis. This finding may show that adjuvant chemotherapy may be beneficial in pN0M0 NSCLC patients with tumors greater than 4 cm in size [8-10].
There are some limitations for this study. First as a prognostic factor on N0M0 patients, tumor extension is not excluded in this study, so it may be a confounding factor on survival analysis. Second, information on adjuvant chemotherapy was not available for this study.
In conclusion, for pN0M0 NSCLC patients, tumor size is an independent prognostic factor. As in the new TNM classification 1 cm increments in tumor size show a good correlation with survival. A tumor size of 4 cm is a significant cut-off point for survival which may help in giving adjuvant chemotherapy decision for N0M0 patients.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Reference
1) Rami-Porta R, Bolejack V, Crowley J, Ball D, Kim J, Lyons G, et al. IASLC Staging and Prognos¬tic Factors Committee, Advisory Boards and Participating Institutions. The IASLC lung cancer staging project: proposals for the revisions of the T descriptors in the forthcoming eighth edition of the TNM classification for lung cancer. J Thorac Oncol 2015; 10: 990-1003.
2) Zhang J, Gold AK, Lin HY, Swisher SG, Xing Y, Lee JJ, et al. Relationship between tumor size and survival in non-small cell lung cancer (NSCLC): an analysis of the surveillance, epidemiology, and end results (SEER) registry. J Thorac Oncol 2015; 10: 682-90.
3) Okada M, Koike T, Higashiyama M, Yamato Y, Kodama K, Tsubota N. Radical sublobar resection for small-sized non–small cell lung cancer: A multicenter study. J Thorac Cardiovasc Surg 2006; 132: 769-75.
4) Sihoe ADL, Van Schil P. Non-small cell lung cancer: When to offer sublobar resection. Lung Cancer 2016; 84: 115-20.
5) Takeda S-i, Fukai S, Komatsu H, Nemoto E, Nakamura K, Murakami M. Impact of large tumor size on survival after resection of pathologically node negative (pN0) non-small cell lung cancer. Ann Thorac Surg 2005; 79: 1142-6.
6) Cangır AK, Kutlay H, Akal M, Güngör A, Özdemir N, Akay H. Prognostic value of tumor size in non-small cell lung cancer larger than five centimeters in diameter. Lung Cancer 2004; 26: 325-31.
7) Zhang Y, Sun Y, Chen H. Effect of tumor size on prognosis of node-negative lung cancer with sufficent lymph node examination and no disease extension. Onco Targets and Therapy 2016; 9: 649-53.
8) Speicher PJ, Gu L, Wang X, Hartwig MG, D"Amico TA, Berry MF. Adjuvant chemotherapy after lobectomy for T1-2N0 non-small cell lung cancer: are the guidelines supported? J Natl Compr Canc Netw 2015; 13: 755-61.



