

2Department of Nuclear Medicine, Medicalpark Hospital Antalya, Turkey
3Department of Hematology and Stem Cell Transplantation Unit, Medicalpark Hospital Antalya, Turkey
4Department of Otolaryngology, Istinye University Health Sciences Faculty, Istanbul, Turkey DOI : 10.26663/cts.2018.0001
Summary
Background: Mediastinal lymphadenopathy (MLAP) is observed in various conditions of malignant or benign diseases. The two common diseases leading to MLAP are mediastinal lymphomas and sarcoidosis. The aim of study is to describe distinctive lymph node involvement patterns with sarcoidosis and lymphoma defined by PET-CT.Materials and Methods: 82 patients (45 women and 37 men) with a median age of 53.5 (21-88) years who had PET-CT for differential diagnose for MLAP were evaluated retrospectively. 31 (37.8%) patients diagnosed sarcoidosis, and 51 (62.2%) lymphoma that had histologically proven by various surgical procedures.
Results: There were no statistical difference between gender, age and average SUV max of groups (p = 0.068, p = 0.846, p = 0.338). 26 of 31 patient (83.9%) of sarcoidosis group had abnormal findings compared the lymphoma group (51.0%) which showed statistically significant difference (p = 0.003). Meanwhile there were no statistical difference between hilar lymph nodes and liver involvement among the groups (p = 0.239 and p = 0.917), cervical, axillary, abdominal lymph nodes and spleen involvement was significantly higher in the lymphoma group (p = 0.008, p < 0.001, p < 0.001 and p = 0.001). Bone marrow (BM) involvement were also significantly higher in lymphoma group (p < 0.001).
Conclusions: There are no specific MLAP findings to differentiate sarcoidosis from lymphomas by PET-CT. It is more likely that the pathological conclusion will be consistent with lymphoma rather than sarcoidosis, in case of involvement of cervical, abdominal and axillary lymph nodes, spleen and BM involvement; however abnormal pulmonary parenchymal findings are in the favor of the diagnosis of sarcoidosis.
Introduction
Mediastinal lymphadenopathy (MLAP) is observed in various conditions during evolution of malignant or benign diseases. The two common diseases leading to MLAP are mediastinal lymphomas and sarcoidosis [1]. Radiologic evaluation is the first step for diagnosis. Plain chest X-ray and computerized tomography (CT) findings are well described in the medical literature for decades [2]. Sarcoidosis preferentially involves bilateral and symmetrical hilar and mediastinal lymph nodes [2,3]. In the advanced stages of the disease, sarcoidosis may also involve pulmonary parenchyma, other lymph nodes or other organs as well [4].Lymphoma is a malignant disorder of lymphatic system, mostly originating from lymph nodes. Hodgkin lymphoma (HL) and Non-Hodgkin lymphoma (NHL) may both involve mediastinal lymph nodes [1,5]. Positron emission tomography with 18-fluorodeoxyglucose (PET-CT) is widely used in differential diagnosis of MLAPs [6]. High FDG uptake levels may be present in both disease, but additional findings are thought to be helpful in differential diagnosis.
The aim of this study is to describe distinctive lymph node involvement patterns among patients with sarcoidosis and lymphoma involving the mediastinum defined by PET-CT.
Methods
Between September 2008 and September 2017, totally 82 patients (45 women and 37 men; median age of 53.5, range 21-88 years) were retrospectively evaluated by PET CT for differential diagnosis of MLAP greater than 1 cm in contrast-enhanced CT, at a single center.The PET-CT was obtained using Discovery ST4 PET-CT fusion system (General Electric Medical Systems, Milwaukee, WI, USA). Following 6 hours of fasting, patients were administered intravenous 18F-FDG (5.2 MBq/kg body weight) and scanning was done 60 minutes later. Three-dimensional PET acquisition and attenuation corrections for CT attenuation maps were carried out. Using the lean body mass-based maximum standardized uptake value (SUV), the SUV max was calculated. PET/CT images were retrospectively interpreted by the same experienced nuclear medicine physician. The SUV max values of above 2.5 were considered as positive for lymph nodes, liver, spleen, and bone marrow involvement. Nodules, infiltration and mass in the lung were considered as parenchyma involvement.
Patients were included into the study who had histologically proven by mediastinoscopy, mediastinotomy, peripheral lymph node biopsy, open surgical procedures, Ultrasound (US) or CT guided core needle biopsy. The biopsy localization was determined according to accessibility with the physical examination and visibility on PET-CT. Lymphoma diagnosed by peripheral lymph node biopsy was 68.6% of all lymphomas, whereas sarcoidosis diagnosed prominently with mediastinoscopy or mediastinotomy (77.45%). Open surgical procedures with general anesthesia such as thoracotomy or laparotomy were performed in 7 (8.5%) patients, and 7 (8.5%) patients were diagnosed via interventional radiologic approach using US or CT guided biopsies (Table 1).
Table 1: Diagnostic procedures according to groups.
Except age and gender, clinical physical examination findings or laboratory data were not analyzed. Mediastinal masses caused other than sarcoidosis or lymphoma, tuberculosis, sarcoid reactions, and metastasis of solid tumors were excluded in this study.
Statistical Analysis
Results were evaluated with SPSS20tm statistical software (SPSS Inc., Chicago, IL, USA). Categorical values were compared with non-parametric Independent Sample t test, and non-categorical values were tested with Pearson chi-square and Fisher exact test. Statistical significance was accepted for the p-value was <0.05.
Results
There was no statistical difference between gender and disease groups (p = 0.068). Mean age of sarcoidosis group was 51.54 (± 13.54) and lymphoma group was 50.54 (± 19.71) without statistical difference (p = 0.846). Average SUV max was 10.14 (± 6.11) in the sarcoidosis group and 8.85(± 5.73) in the lymphoma group without a statistically significant difference (p = 0.338) (Table 2).Table 2: Demographic features.
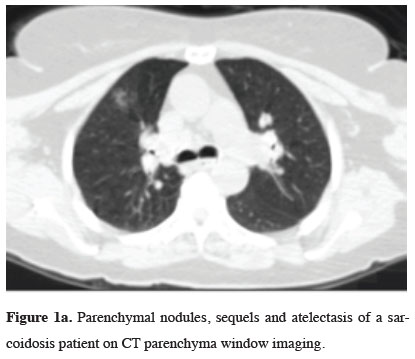
Analysis of PET-CT findings apart from the mediastinal region is summarized in Table 3. When pulmonary parenchymal findings evaluated, 26 of 31 patients (83.9%) of sarcoidosis group had abnormal findings compared the lymphoma group (51.0%) which showed statistically significant difference (p = 0.003). (Figure 1a).
 Click Here to Zoom |
Figure 1a: Parenchymal nodules, sequels and atelectasis of a sarcoidosis patient on CT parenchyma window imaging. |
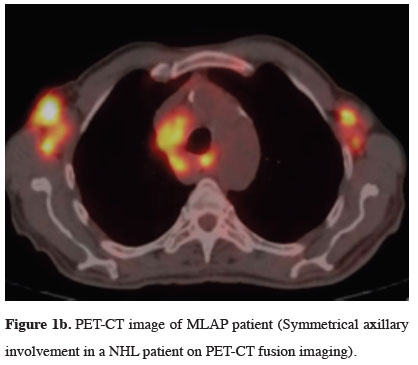
When hilar lymph nodes were evaluated, there were no statistical difference in involvement among the patient groups (p = 0.239). When cervical, axillary and abdominal lymph nodes were compared, it was commonly observed in the lymphoma group with statistically significance (p < 0.008, p < 0.001, and p < 0.001 respectively) (Figure 1b).
 Click Here to Zoom |
Figure 1b: PET-CT image of MLAP patient (Symmetrical axillary involvement in a NHL patient on PET-CT fusion imaging). |
When liver and spleen involvement were evaluated, although there was no difference was observed in terms of hepatic involvement (p = 0.917), spleen involvement was significantly higher in the lymphoma group (p = 0.001) (Figue 1c).
 Click Here to Zoom |
Figure 1c: Cervical, axillary lymph nodes and splenic involvement in a NHL patient on PET-CT. |
BM involvement determined by PET-CT were also significantly different between the two groups favoring the patients with lymphoma (p < 0.001) (Table 3).
Discussion
MLAP is observed in several inflammatory, infectious or malignant diseases. It is important to diagnosis and differentiate benign from malignant conditions. Most common malignant etiology is mediastinal lymphoma, whereas common benign disease is sarcoidosis [1].Sarcoidosis is a multisystem granulomatous disorder of unknown etiology, characterized by noncaseating granulomas in preferentially involves bilateral and symmetrical hilar and mediastinal lymph nodes [3,7]. Duration of disease, sarcoidosis may also involve less commonly cervical lymph nodes, lung parenchyma, liver, spleen, eyes, kidneys and heart as well as thyroid glands [4,8].
Lymphoma is a malignant disorder of lymphatic system, mostly originating from lymph nodes. Hodgkin lymphoma (HL) and Non-Hodgkin lymphoma (NHL) may both involve mediastinal lymph nodes. In our series 12 (23.5%) of the patients were HL, and 39 (76.5%) of them were NHL similar to the rates reported in the literature [1,2,5].
Although tuberculosis-associated MLAP is usually seen in the primary infection complex in childhood, it can be seen in adults in endemic region and immunocompromised or HIV patients. Pulmonary findings are predominantly found in adult tuberculosis patients and diagnosed with microbiologic methods regardless of biopsy in general [9,10]. In our 9-years" experience, we only encountered 9 adult patients with tuberculosis depended MLAP.
Thoracic radiologic examination is the first step in differential diagnosis. Chest X-ray and CT findings are well described in both conditions. CT has low sensitivity (64%) and specificity (62%) in detecting malignant lymph nodes [2]. PET-CT is widely used in differential diagnosis of MLAP increasingly for last two decades [2,5,11].
The SUV max levels cannot differentiate sarcoidosis from malignancy, as PET-CT may be positive in both [6,11-13]. In our study, sarcoidosis patients" average level of SUV max was 10.14 (± 6.11), meanwhile lymphoma was 8.85 (± 5.73) with no statistical difference (p = 0.338).
In patients with sarcoidosis, parenchymal findings in the lungs are variable and pulmonary manifestations may occur in up to 90% of cases. Chest radiographic findings may be observed in advanced stages. Stage IV disease is characterized by reticular opacities with evidence of volume loss predominant in the upper zones of the lungs [2,3,7]. In our study, 83.9% of sarcoidosis patient had parenchymal findings versus 51.0% in the lymphoma group which showed statistically significant difference (p = 0.003) (Figure 1c).
Bilateral hilar symmetrical lymphadenopathy is a classic radiologic finding in sarcoidosis [2,3,7]. Hilar lymph node involvement is also common in the lymphoma and more frequent in HL (85%) and in about half of NHL. HL most commonly involves anterior and superior mediastinal nodes, pre-vascular and para-tracheal lymph nodes are also affected [5,13]. In our study, hilar lymph nodes were involved 87.1% in sarcoidosis and 76.5% lymphoma group, without statistically significant difference between groups (p = 0.239).
In HL, mediastinal involvement is present in 60% of patients at the time of diagnosis whereas the disease is limited to mediastinum only in 3% of cases. In patients with NHL a higher percentage of mediastinal involvement is observed compared to (10-20%) HL, which may be present either as the sole involvement (e.g., primary mediastinal large B cell lymphoma) or as part of systemic disease [3,5,14]. PET-CT is highly sensitive and specific for detecting NHL in nodal and extra nodal sites [14]. Additional LN involvement patterns in areas other than mediastinal region may help differential diagnosis among lymphoma and sarcoidosis [6,8,14] (Figure 1a,b).
Even though peripheral lymph node involvement determined by PET-CT is not common and specific for sarcoidosis, it may be helpful for identify occult or coincidental sites and diagnostic accessibility when observed [6,12,15]. In our study, 4 (12.9%) of sarcoidosis patients had undergone peripheral lymph node biopsy to avoid invasive surgery requiring general anesthesia.
Spleen involvement by lymphoma generally presents either diffuse involvement with higher uptake compared to liver or solitary / multiple nodules in splenic parenchyma determined by PET-CT. Besides of the size which does not correlate with involvement, spleen is affected in one third of all lymphomas [16,17]. In this study, splenic involvement was found to be significantly higher in the lymphoma group compared to the sarcoidosis group (41.2% vs 6.5%, p = 0.001).
Bone marrow involvement is found in approximately 50% to 80% of patients with low grade NHL, 25% to 40% of high-grade NHL, and 5% to 14% of HL during the time of diagnosis [18,19]. In a meta-analysis that included data from seven studies with 654 patients with newly diagnosed NHL, PET had moderate sensitivity (88.7 %) and high specificity (99.8 %) for the detection of BM involvement [19]. Thus, for patients with NHL, normal BM on PET scan does not rule out presence involvement, but, FDG uptake in BM is highly specific for involvement with lymphoma [18,19]. As PET-CT is not routinely used for the diagnosis of sarcoidosis, there is no correct data about BM involvement rates yet. Yanardag and de Prost reported that, BM involvement must be suspected in case of anemia in a sarcoidosis patient [20,21]. In our study, BM involvement determined by PET-CT was significantly different between the two groups favoring the patients with lymphoma (p < 0.001).
In the literature, although PET-CT findings of MLAP due to lung cancer, metastatic diseases, sarcoidosis, tuberculosis, and lymphoma was separately investigated, a study comparing sarcoidosis and lymphoma findings has not published yet before this study to our knowledge.
Our study has a limitation; none of the diagnoses was made with endobronchial ultrasound guided trans-bronchial biopsy.
In conclusion, sarcoidosis and lymphoma are the common causes of MLAPs that may both involve hilar and mediastinal lymph nodes. There are no specific findings to differentiate sarcoidosis from lymphomas by PET-CT. However, lymph node involvement patterns, spleen and BM invasion may help for differential diagnosis and define biopsy procedure. It is more likely that the pathological conclusion will be consistent with lymphoma rather than sarcoidosis in case of involvement of cervical, axillary and abdominal lymph nodes, spleen, and BM by PET-CT, however, abnormal pulmonary parenchymal findings are in favor of diagnosis of sarcoidosis.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest 2005; 128: 2893-909.
2) Gurney JW. Mediastinum. In Gurney JW, Winer-Muram H, Stern EJ Editors Diagnostic Imaging Chest. Salt Lake City, Utah, USA: AMIRSYS; 2006 p: 107-9.
3) Diem Quan Hoang, Elsie T. Nguyen, Sarcoidosis. Seminars in Roentgenology, January 2010 Volume 45, Issue 1, p: 36- 42.
4) Ozkan Z, Oncel M, Kurt N, Kargi AB, Ozdemir N, Kaptanoglu L et al. Sarcoidosis presenting as cold thyroid nodules: report of two cases. Surg Today 2005; 35: 770-3.
5) North LB, Libshitz HI, Lorigan JG. Thoracic lymphoma. Radiol Clin North Am 1990; 28: 745-62.
6) Kumar A, Dutta R, Kannan U, Kumar R, Khilnani GC, Gupta SD. Evaluation of mediastinal lymph nodes using F-FDG PET-CT scan and its histopathologic correlation. Ann Thorac Med 2011; 6: 11-6.
7) Larici AR, Glaudemans AW, del Ciello A, Slart RH, Calandriello L, Gheysens O. Radiological and nuclear medicine imaging of sarcoidosis. Q J Nucl Med Mol Imaging 2018; 62: 14-33.
8) Okumus G, Musellim B, Cetinkaya E, Turker H, Uzaslan E, Yenturk E, et al. Extrapulmonary involvement in patients with sarcoidosis in Turkey. Respirology 2011; 16: 446-50.
9) Bhalla AS, Goyal A, Guleria R, Gupta AK. Chest tuberculosis: radiological review and imaging recommendations. Indian J Radiol Imaging 2015; 25: 213-25.
10) Pirina P, Spada V, Santoru L, Polo MF, Molicotti P, Marras V et al. Chest tuberculosis with mediastinal asymptomatic lymphadenitis without lung involvement in an immunocompetent patient. J Infect Dev Ctries 2013; 7: 280-5.
11) Hyun Jung Koo, Mi Young Kim, So Youn Shin, Sooyoung Shin, Sung-Soo Kim, Sei Won Lee, Chang-Min Choi. Evaluation of Mediastinal Lymph Nodes in Sarcoidosis, Sarcoid Reaction, and Malignant Lymph Nodes Using CT and FDG-PET/CT. Medicine (Baltimore) 2015; 94: e1095.
12) Treglia G, Annunziata S, Sobic-Saranovic D, Bertagna F, Caldarella C, Giovanella L. The Role of 18F-FDG-PET and PET/CT in Patients with Sarcoidosis: An Updated Evidence based Review. Academic Rad 2014; 21: 675-84.
13) Hutchings M, Loft a, Hansen M, Pedersen LM, Berthelsen AK, Keiding S, et al. Position emission tomography with or without computed tomography in the primary staging of Hodgkin"s lymphoma. Haematologica 2006; 91: 482-9.
14) Paes FM, Kalkanis DG, Sideras PA, Serafini AN. FDG PET/CT of extranodal involvement in non-Hodgkin lymphoma and Hodgkin"s disease. Radiographics 2010; 30: 269-91.
15) Teirstein AS, Machac J, Almeida O, Lu P, Padilla ML, Iannuzzi MC. Results of 188 wholebody fluorodeoxyglucose positron emission tomography scans in 137 patients with sarcoidosis. Chest 2007; 132: 1949-53.
16) Saboo S S, Krajewski K M, O"regan K N, Giardino A, Brown J R, Ramaiya N, Jagannathan J P, Spleen in haematological malignancies: spectrum of imaging findings. Br J Rad 2012; 85: 81-92.
17) Strijk SP, Boetes C, Bogman MJJ T, De Pauw BE & Wobbes Th. The Spleen in Non-Hodgkin Lymphoma, Acta Radiologica 1987; 28: 139-44.
18) Adams HJ, Nievelstein RA, Kwee TC. Opportunities and limitations of bone marrow biopsy and bone marrow FDG-PET in lymphoma. Blood Rev 2015; 29: 417-25.
19) Carr R, Barrington SF, Madan B, O"Doherty MJ. Detection of Lymphoma in Bone Marrow by Whole-Body Positron Emission Tomography. Blood 1998; 91: 3340-6.



