

2Kartal Kosuyolu Heart & Research Hospital, Thoracic Surgery, Istanbul, Turkey DOI : 10.26663/cts.2018.0003
Summary
Congenital lobar emphysema (CLE) is a rare developmental anomaly of the lower respiratory tract, which generally presents during the neonatal/pediatric period. Lobectomy is the only curative treatment for CLE. An 18-year-old male with enlarging left anterior chest wall deformity and progressive breathlessness for the last 2 years admitted to our clinic.Physical examination revealed asymmetrical expansion of left hemithorax. Chest radiography and thoracic computed tomography demonstrated hyperinflation of the left upper lobe and a mediastinal shift to the right side. FEV1 was 1.70 L (50%). Ventilation-perfusion scintigraphy showed reduced perfusion and ventilation in the right lung to 33.4% (upper zone, 1.9%; middle zone, 10.0%; lower zone, 22.5%). Patient underwent a successful video-assisted thoracoscopic surgery (VATS) left upper lobectomy, and was discharged on postoperative day 5. He is still being followed-up on fifth year, asymptomatically, with normalized chest wall appearance. VATS lobectomy is a feasible, safe and effective treatment for congenital pulmonary disorders, even for delayed cases.
Introduction
Congenital lobar emphysema (CLE) is a rare developmental anomaly of the lower respiratory tract characterized by over-inflation of one or more pulmonary lobes [1]. Its etiology is unknown. CLE is usually diagnosed in the neonatal period and early childhood. It is almost always unilateral with a male dominance [1,2]. Its curative management has traditionally been surgical.Interestingly, the present report describes an adult with symptomatic CLE diagnosed at the age of 18 years, and treated with a minimally invasive surgical approach.
Case Presentation
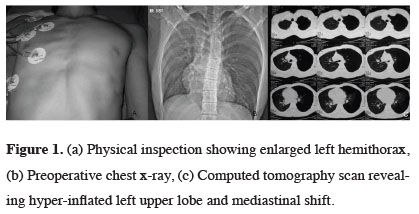
An 18-year-old man with gradual onset of mild breathlessness and expansion of left anterior chest wall, for the last 2 years, admitted to our clinic. There was no history of cyanosis, jaundice, convulsion, or heart failure. Physical inspection showed an expanded left hemithorax. On cardiovascular system examination, the heart sounds were shifted to the opposite side. No gross cardiac anomaly was found. Chest radiography and thoracic computed tomography (CT) demonstrated hyperinflation of the left upper lobe and a mediastinal shift to the right side (Figure 1). Pulmonary function tests revealed restriction by forced vital capacity 2.18 L (51%) and forced expiratory volume in first second 1.70 L (50%). Ventilation-perfusion scintigraphy showed reduced perfusion and ventilation in the right lung to 33.4% (upper zone, 1.9%; middle zone, 10%; lower zone, 22.5%). Fiberoptic bronchoscopic examination confirmed the absence of an endobronchial lesion.
 Click Here to Zoom |
Figure 1: (a) Physical inspection showing enlarged left hemithorax, (b) Preoperative chest x-ray, (c) Computed tomography scan revealing hyper-inflated left upper lobe and mediastinal shift. |
After receiving an informed consent from the patient, VATS lobectomy was planned. The patient was placed in a lateral decubitus position and single lung ventilation was achieved. A tree-port thoracoscopic lobectomy was performed through a 4cm utility incision without using a rib retractor. Space restrictions added difficulty to the procedure, as the distended nondeflated lung lobe left too little room for the surgeon to achieve adequate manoeuvres, the resection was successfully completed without conversion to thoracotomy.
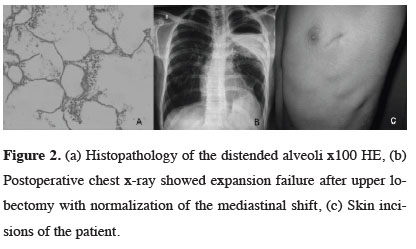
Histopathological examination revealed distended alveoli and elongated cystic spaces, consistent with CLE (Figure 2a). Postoperative chest X-ray showed inadequate expansion of the remaining lobe due to prolonged compression (Figure 2b). However, no clinical signs or symptoms were occurred and he was discharged on postoperative day 5. He is still being followed-up on fifth year, asymptomatically, with a small utility incision (Figure 2c).
 Click Here to Zoom |
Figure 2: (a) Histopathology of the distended alveoli x100 HE, (b) Postoperative chest x-ray showed expansion failure after upper lobectomy with normalization of the mediastinal shift, (c) Skin incisions of the patient. |
Discussion
CLE has a prevalence of approximately 1:20,000 to 1:30,000 and was first identified in 1932 by Nelson [1-5]. Gross and Lewis declared the first successful surgical repair [6]. Typically, a single lobe on one side is affected but multi-lobar involvement may occasionally occur. Most frequently affected sites are the left upper, right middle and upper lobes, respectively [2]. Our case was 18- year old male and he had left upper lobe CLE.Clinical presentation varies from acute neonatal respiratory failure to chronic recurrent episodes of tachypnea or infections [3]. Late manifestation is unusual; adults often present with dyspnea, infection or cough. In infancy, it usually arises as respiratory distress. Progressive hyperinflation of a lobe or lobes results in compression atelectasis, mediastinum shift, impaired venous cardiac return, secondary hypoxia, and hypotension. In our case the patient had mild shortness of breath.
The etiology of CLE is unknown, and in 50% of cases no specific cause was found [7]. It is likely that abnormal interactions between embryonic endodermal and mesodermal components of the lung during bronchopulmonary development lead to progressive lobar hyperinflation [5]. The current theory, which suggests inadequate cartilaginous support of the bronchus, was first proposed by Gross and Lewis [8]. However, a preferred theory is based on a recently described pathological entity called the polyalveolar lobe, caused by a 3 to 5 fold increase in the number of alveoli in the whole lobe [9]. More commonly, in 25% of cases, a congenital defect of cartilage and bronchial obstructions are encountered. In another 25%, the development of CLE is caused by bronchial obstruction. Reports showed an association of CLE with other congenital diseases as heart failure and various cardiac defects [7].
Clinical diagnosis of congenital lobar emphysema is difficult and requires perception. Anterior-posterior and a lateral chest radiograph view provides vital information, but not definitive. The characteristic appearance is a hyper-inflated lobe with compression to adjacent lobes. The vascular supply to the emphysematous lobe is poor and vascular markings in the affected lobe are vanished, but maintained on the periphery of the lung [1]. In contrast to pneumothorax, there is no line of pleural demarcation. Widening of the rib spaces and depression of the diaphragm on the affected side is as seen in Figure 1. The mediastinum may be displaced away from the emphysematous side. In severe cases, the over-expanded lung may herniate into the contralateral hemithorax [1,6]. A scintigraphic scan depicts ventilation defects and decreased perfusion in the hyper-expanded lobe due to decreased vascularity [9]. Computed tomography scan of our patient revealed hyper-inflated left upper lobe and mediastinal shift.
The curative treatment of CLE in symptomatic patients is surgical resection by either thoracotomy or using a thoracoscopic approach. Greatest risk of surgery is on induction of anaesthesia i.e. if positive pressure ventilation is applied before opening of the chest, it may cause rapid inflation of the emphysematous lobe or cyst, resulting in a sudden mediastinal shift and cardiac arrest. Therefore, induction of anaesthesia should provide adequate spontaneous ventilation with minimal airway pressure and intermittent manual assistance is essential. Three-portal VATS using single-lung ventilation was performed in the present case. The anterior port was enlarged to 4 cm and instruments were used through this site without a rib retractor. The major difficulty of performing thoracoscopic resection on an emphysematous lobe is the huge intrathoracic area occupied by the nondeflated lobe, while vascular structures are easy to manage with endoclips.
As a conclusion, even though CLE is rare, clinical awareness of this condition is important for early diagnosis and effective surgical treatment. For a certain subgroup of patients, VATS lobectomy can be a safe and effective treatment for congenital pulmonary disorders, despite late diagnosis or physical complication occurrence.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Tempe DK, Virmani S, Javetkar S, Banerjee A, Puri SK, Datt V. Congenital lobar emphysema: Pitfalls and management. Ann Card Anaesth 2010; 13: 53-8.
2) Sadaqat M, Malik JA, Karim R. Congenital lober emphysema in an adult. Lung India 2011; 28: 67-9.
3) Thakral CL, Maji DC, Sajwani MJ. Congenital lobar emphysema: experience with 21 cases. Pediatr Surg Int 2001; 17: 88-91.
4) Mei-Zahav M, Konen O, Manson D, Langer JC. Is congenital lobar emphysema a surgical disease? J Pediatr Surg 2006; 41: 1058-61.
5) Nelson RL. Congenital cyctic disease of the lung; report of case. J Pediatr 1932; 1: 233-8.
6) Kennedy CD, Habibi P, Matthew DJ, Gordon I. Lobar emphysema: Long term imaging follow up. Radiology 1991; 180: 189-93.
7) Calıskan T, Okutan O, Ciftci F, Kartaloglu Z, Tas D, Demirer E. Congenital Lobar Emphysema Diagnosed in Adult Age: A Case Report. Eurasian J Pulmonol 2014; 16: 50-3.
8) Gross RE, Lewis JE, Jr. Defect of anterior mediastinum.Succesful surgical repair. Surg Gynecol Obstet 1945; 80: 549-54.
9) Celiksoy MH, Sogut A, Sancak R, Koken O. Congenital lobar emphysema. Abant Med J 2014; 3: 289-92



