

2Department of Radiology, Private Medstar Antalya Hospital, Antalya, Turkey
3Department of Anesthesiology and Reanimation, Private Medstar Antalya Hospital, Antalya, Turkey
4Department of Medical Oncology, Private Medstar Antalya Hospital and Memorial Antalya Hospital, Antalya Turkey DOI : 10.26663/cts.2018.0005
Summary
Upper airway obstructions with malignant or benign causes have high mortality and morbidity rates and may lead to sudden respiratory distress. Head-neck tumors, cervical esophagus tumors, longterm intubation, and tracheostomies can lead to airway obstruction. Four cases (one with a long-term intubation tracheomalacia and three with malignant upper airway obstructions) that tracheostomy had been inadequate and performed tracheal stomal stent application were presented with literature. These cases show that tracheal stoma stents are an effective method for providing airway palliation and increasing quality of life.Introduction
Upper airway obstructions with malignant or benign causes have high mortality and morbidity rates and may lead to sudden respiratory distress [1]. Surgery is the primary treatment for airway obstructions and fistulas for head-neck tumors and cervical esophagus tumors [1-5]. When surgery is not possible, airway continuity is provided by tracheostomy; however, in some cases tracheostomies are inadequate for keeping the airway open due to involvement of the distal part of the trachea. Here we present case studies of 4 patients in whom tracheal stomal stents (TSS) were placed.Case Presentation
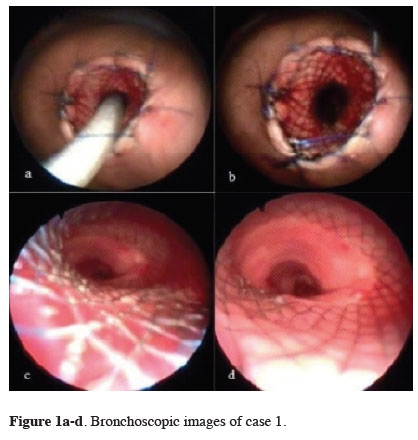
Case 1A 40-year-old female patient underwent a tracheostomy due to cervical esophagus carcinoma. The patient was undergoing radiochemotherapy and was evaluated for a complaint of respiratory distress. In the computed tomography (CT) examination, progressing tumor tissue was observed in the cervical region and a stenosis that had progressed until the end of the tracheostomy canula was observed in the trachea. Bronchoscopy revealed the presence of a tumor leading to airway obstruction, therefore, a TSS (80 mm partial-coated, 20 mm diameter) was placed under sedation over the carina to the tracheostomy stoma. The start of the stent was fixed to the stoma via polypropylene suture (Figure 1). The patient died on the 45th day with disease progression.
 Click Here to Zoom |
Figure 1a-d: Bronchoscopic images of case 1. |
Case 2
A 62-year-old male patient undergoing radiochemotherapy for a head-neck tumor complained of respiratory distress and underwent a tracheostomy. Upper gastrointestinal endoscopy revealed a tracheo-esophageal fistula (TOF). A stent had been previously placed in the esophagus. Progressing tumor tissue was observed in the cervical region and stenosis, which had progressed to the end of the tracheostomy, was observed in the trachea. The bronchoscopy revealed a stenosis in the trachea and a 3-cm sized TOF at the back wall of the trachea. A TSS (80 mm partial coated stent with a 20 mm diameter) was placed under sedation to the tracheostomy stoma over the carina (Figure 2). The procedure resulted in mitigation of respiratory distress and provided a clear airway during 175 days.
 Click Here to Zoom |
Figure 2a-c: Thorax CT images of case 2, d. stoma image of same case. |
Case 3
A 72-year-old male patient receiving radiochemotherapy for larynx carcinoma was evaluated for respiratory distress and subsequently underwent a tracheostomy. Progressing tumor tissue was observed in the cervical region with CT, as well as a stenosis in the trachea that had progressed 3 cm over the carina. Bronchoscopy revealed tumor invasion and a stenosis starting in the stoma and progressing until the mid-trachea following a tracheostomy. Under sedation, a TSS (80 mm partial coated stent with a 20 mm diameter) was placed until the tracheostomy stoma was over the carina. There was a significant reduction in respiratory distress and no problems during 33 days.
Case 4
A 60-year-old male patient who received a tracheostomy 19 years ago due to a vehicle accident, followed by home-care services on a ventilator, and was evaluated for respiratory distress. The patient had a restricted airway despite an adjustable special tracheostomy cannula, and thorax CT imaging revealed that the diameter of the trachea was as large as 6 cm. Approximately 4 cm TOF was detected via upper gastrointestinal endoscopy. Bronchoscopy revealed reduced vocal cord movements and significant tracheomalacia starting at the tracheostomy cannula. The 2 cm of the trachea exceeding the carina was healthy. A 120x22 mm partially coated esophagus stent was placed under sedation, followed by placement of a TSS (140 mm partial coated stent with a 22 mm diameter) over the carina, reaching the tracheostomy stoma under the guidance of a fiberoptic bronchoscope. To avoid any shifts, the stent was fixed to the stoma with polypropylene sutures and fixed with a tracheostomy cannula (Figure 3). During 105 days, the patient was then connected to a ventilator without any issues.
 Click Here to Zoom |
Figure 3a,b,d: Thorax CT images of case 4, c. bronchoscopic image of the distal trachea. |
Surgical Technique
The patients were evaluated via head-neck tomography and thorax CT. The localization of the stenosis and normal sizes of the trachea were noted, and the localization of the stenosis and TOF and status of the left and right bronchial systems were determined by a fiberoptic bronchoscope prior to the procedure. Finally, the proper stent was selected (Metallic, partially coated, "self-expandable" stents (M.I.Tech Co. Ltd, Gyunggi -do, Korea). The procedure was performed in an operating room under sedation and local anesthesia. The stent system was placed compromising the 2 cm healthy part of the distal trachea under the guidance of fiberoptic bronchoscopy, the cover on the stent system was pulled back, and the TSS was placed at the proximal part touching the stoma. The stoma was fixed by prolene surrounding sutures to avoid displacement (Figures 1, 2).
Discussion
In upper airway pathologies, symptoms depend on the additional pulmonary pathologies that accompany the localized obstruction of the airway. Initially, coughing and exertion increase respiratory effort, and subsequently respiratory distress is observed while resting. Sudden respiratory failure may be observed with secretions and accompanying infections [3]. A history of aspiration, severe cough, and unmanageable pneumonia may suggest TOF [6]. Physical exams reveal the presence of stridor, low oxygenation, wheezing sounds, and noisy respiratory sounds. Test results indicating impaired respiratory function and blood gases aid in diagnosis. Cervical and thorax CT determine the localization and length of the pathologies, as well as any pressure from the external regions or intraluminal pathology. Gafaar et al. [7] reported using "multi-slice" tomography, 3-dimensional reconstruction, and virtual bronchoscopy of the neck and thorax in pre-operative evaluation. Bronchoscopy is a standard diagnostic and treatment method using invasive procedures. All of our cases had previous tracheostomies, cervical CT, thorax CT and fiber optic bronchoscopy were performed to clarify the underlying cause(s) of respiratory distress.Tracheal stents are indicated for stenosis or obstructions caused by external pressures; in the presence of greater than 50% stenosis after laser or brachytherapy, TOF, primary or post-operational tracheomalacia, and in patients not suitable for surgery [1,2,8-10]. Tracheostomy is another method for providing an open airway in cases not suitable for tracheal stents. TSS is another method used to provide an open airway when a standard tracheal stent is not appropriate and tracheostomy is inadequate [11]. The objectives here were to correct the airway obstruction related to progressing local tumor tissue via a stent, increase the quality of life, and avoid airway obstruction [10]. For 3 of the 4 cases considered here, the Montgomery T tube was not an alternative since there was no proximal airway; in the remaining case, TSS was preferred based on accompanying TOF, long-segment tracheomalacia secondary to tracheostomy, and the need for ventilator support.
TSS is preferred in cases not suited for a standard tracheal stent, such as trachea stenosis, TOF, and tracheomalacia [11]. Only Spelsberg et al. [11] has reported an application of TSS for TOF in 6 laryngectomized cases, which is the same type of case as ours. The TSS applications defined by Samuel Garcia et al. [12] and Hall et al. [13] are not exact matches to our application.
Consecutive or concomitant stent placement into the trachea or esophagus is particularly recommended in the presence of TOF [6]. However, this method has the disadvantage of fistula widening due to necrosis in healthy tissue that is exposed to pressure [1]. For our two TOF cases, the esophagus was stented first followed by the application of a TSS. This provides back-support for the stent placed into the trachea within the mediastinum, prevents displacement, and avoids closing of the fistula. In this case, stenting of the esophagus or trachea should be planned based on the location of the fistula.
Tracheomalacia is another indication for TSS [3,9]. Stent placement is indicated in multiple long-segment malacias, although there are no constant areas of stenosis [1]. The most important issue in cases with tracheomalacia is the prevention of stent displacement [3,9,15]. Patient selection must include screening for limited malacia and the presence of healthy tissue in the distal regions [3]. In one of our cases, TSS was performed due to post-tracheostomy tracheomalacia. Here, a long-term tracheostomy with cuff led to tracheomalacia. The most important problems were displacement of the silicone or metal stent and fixation to prevent leakage from its surroundings and some methods were reported for fixation [3,14,15]. Our case did not require additional fixation since we believed that the stent placed in the distal trachea was fixed in the environment and covered with 2 cm of healthy tracheal tissue. However, air leakage was observed through the TOF area after the procedure, but ventilation of the patient was not impaired. Here, the fixation of TSS at the tracheal end via thoracotomy is preferred due to the decreased risk of morbidity.
Metal and silicone stents are the most commonly used tracheal stents. Metals stents are preferred to silicone stents since they are more effective at opening the areas of stenosis, more compatible with the anatomy, provide better mucociliar cleaning, and lead to less bacterial colonization and migration [1,7,8]. Partial coated, "self-expandable" metallic stents were used as TSS in our 4 cases based on the considerations mentioned above.
The complications of stents are migration, spitting out of the stent while coughing, erosion to the surrounding tissues, bleeding, difficulty swallowing, chest pain, secretion accumulation, granulated tissue development, obstructions, bad breath, infection, and stent breakage [2,3,7-
Declaration of conflicting interests
Funding
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
The authors received no financial support.
Reference
1) Shin JH, Song H, Shim TS. Management of tracheobronchial strictures. Cardiovasc Intervent Radiol 2004: 27; 314-24.
2) Serano C, Laborda A, Lozano JM, Caballero AS, Lopera J, Gregoria, MA. Metallic stents for tracheobronchial pathology treatment. Cardiovasc Intervent Radiol 2013; 36: 1614-23.
3) Bacon JL, Patterson CM, Madden BP. Indications and interventional options for non-resectable tracheal stenosis. J Thorac Dis 2014; 6: 258-70.
4) Nair S, Mohan S, Mandal G, Nilakantan A. Tracheal stenosis: our experience at a tertiary care centre in India with special regard to cause and management. Indian J Otolaryngol Head Neck Surg 2014; 66: 51-6.
5) Vandemoortele T, Laroumagne S, Bylicki O, Astoul P, Dutau H. Endobronchial treatment of complete tracheal stenosis: report of 3 cases and description of an innovative technique. Ann Thorac Surg 2013; 95:351-4
6) Ke M, Wu X, Zeng J. The treatment strategy for tracheoesophageal fistula. J Thorac Dis. 2015; 7 (Suppl 4): S389-97.
7) Gaafar AH, Shaaban AY, Elhadidi MS. The use of metallic expandable tracheal stents in the management of inoperable malignant tracheal obstruction. Eur Arch Otorhinolaryngol 2012; 269: 247-53.
8) Remacle M, Lawson G, Jamart J, Keghian J. Progressive experience in tracheal stenting with self-expendable stents. Eur Arch OtoRhinolaringol2003; 260: 369-73
9) Ozdemir C, Sökücü SN, Karasulu L, Altın S, Dalar L. Tracheomalacia treatment using a large-diameter, custom-made airway stent in a case with mounier-kuhn syndrome. Case Rep Pulmonol 2014; 2014: 910135.
10) Saito Y, Imamura H. Airway stenting. Surg Today. 2005; 35: 265-70.
11) Spelsberg FW, Wollenberg B, Weidenhagen R, Lang RA, Winter H, Jauch KW et al. Tracheal stent for esophagotracheal fistula in laryngectomy patients. Safe fixation to the tracheostoma. HNO. 2009; 57: 1065-9.
12) Garcia S, Gimferrer JM, Iglesias M, Catalan M, Martinez E, Macchiarini P. Self-made tracheal stomal stent using a tracheal T-tube. Ann Thorac Surg 2006; 82: 1545-6.
13) Hall AM, Watt JW. The use of tracheal stoma stents in high spinal cord injury: a patient-friendly alternative to long-term tracheostomy tubes. Spinal Cord 2008; 46: 753-5.



