

2Department of Thoracic Surgery, Dr. Suat Seren Chest Diseases and Thoracic Surgery Training Hospital, İzmir, Turkey DOI : 10.26663/cts.2018.0006
Summary
Penetrating chest traumas constitute nearly one third of all chest traumas with a high high mortality and morbidity. Herein we present a 29-year-old male patient presented at the emergency department with a the penetrating thoracic trauma with a dagger. The management was reported in the light of relevant literatüre.Introduction
Penetrating chest traumas constitute 30% of all chest traumas and they have high mortality and morbidity hence the organs in thorax are vitally important [1,2]. Therefore, the hemodynamics of the cardiorespiratory system should rapidly be corrected and treated.Herein we present a penetrating thoracic trauma due to a dagger wound.
Case Presentation
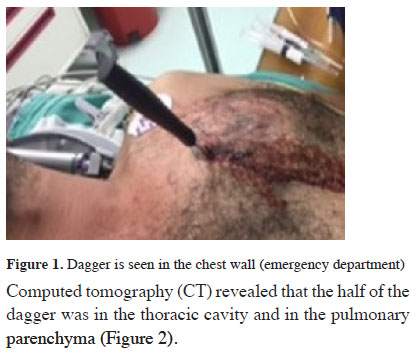
A 29-year-old male patient was admitted to the emergency department due to a stab wound to his chest. He was drunk, wandering around despite the security guards with a dagger on his chest, and refused to lay down at the beginning. He was calmed down and persuaded for examination. On inspection, it was observed that the dagger was on the third anterior intercostal space of the left hemithorax (Figure1). Vital signs were stable at the moment.
 Click Here to Zoom |
Figure 1: Dagger is seen in the chest wall (emergency department) |
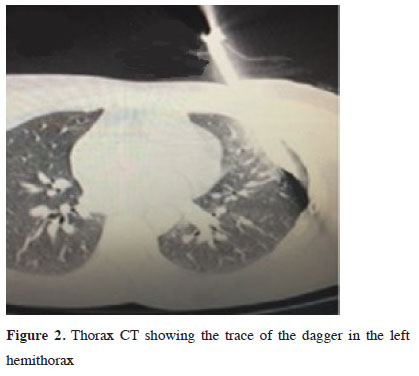
Computed tomography (CT) revealed that the half of the dagger was in the thoracic cavity and in the pulmonary parenchyma (Figure 2).
 Click Here to Zoom |
Figure 2: Thorax CT showing the trace of the dagger in the left hemithorax |
Laboratory results were stable, and he underwent surgery under urgent conditions. A mini posterolateral thoracotomy, preserving the serratus anterior muscle was performed. The dagger was removed from the lung parenchyma in a controlled manner (Figure 3).
 Click Here to Zoom |
Figure 3: The appearance of dagger after removal |
The laceration at the lung parenchyma was repaired primarily. There was no vascular and cardiac injuries. Post operative follow-up was uneventful and he was discharged on the 3rd day of hospitalization.
Discussion
Penetrating trauma to the chest usually causes pneumothorax, hemothorax, hemopneumothorax and diaphragmatic injury. Widened mediastinum indicates injury to the vascular structures and hemopericardium. It is mostly seen in young adult group than children and the elderly. Since young people represent the active and productive age, these injuries causes significant economic and social loss [3-6]. In addition, penetrating chest traumas are most commonly seen in the male population as weapons and sharpening tools can be used and supplied more easily by men then women [5]. Robison et al [7] reported 32.8% gunshot injuries and 67.2% penetrating injuries in a series of 1168 cases. A normal sized knife caused most of the penetrating wounds. In our case it was a dagger and appalling. Although there is a consensus on when and where foreign body should be removed, we think that this issue should be discussed. Many handbooks properly warn against the removal of these sharp tools during the transfer of the patient. Molnar [8] emphasizes that patients are transferred from long distances with a strange foreign body in their chest, and the sharp edges of indwelling objects inevitably rub and cut the surrounding parenchyma. In our patient the dagger was moving synchronously with the heart beat and respiratory movements. Molnar [8] also says that extraction of knives after insertion of a chest drain may be evaluated as alternative to the present protocol.The most common intrathoracic pathologies in penetrating chest trauma are hemothorax, pneumothorax and hemopneumothorax. Two different studies conducted in our country supported this finding [3,4]. Pulmonary parenchymal laceration is also common in penetrating chest trauma. In patients requiring a surgical treatment, laceration is usually repaired with primary sutures. However, resection varies from wedge resection to pneumonectomy in cases of major vessel injury, bronchial injury, or large lacerations that cannot be repaired [9,10]. In our case, primary repair of parenchymal laceration was sufficient although the view was terrifying no major vessel injury or bronchial injury was noted. As a conclusion, penetrating chest injuries generally look smaller in the first sight but majority of them are fatal due to vital organ and major blood vessel injuries. Patients with penetrating chest trauma should be treated promptly under monitorization, and an urgent operation should be performed warrantably.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Graeber GM, Prabhakar G, Shields TW. Blunt and penetrating injuries of the chest wall, pleura, and lungs. In: Shields TW, editor. General thoracic surgery. 6th ed. Philadelphia: Lippincott Williams and Wilkins; 2005. p. 951-71.
2) Yüksel M, Laçin T. Travmalı hastaya yaklaşım. In: Yüksel M, Çetin G, editörler. Toraks travmaları. İstanbul: Turgut Yayıncılık; 2003. s. 1-14.
3) Tekinbaş C, Eroğlu A, Kürkçüoğlu IC, Türkyilmaz A,Yekeler E, Karaoğlanoğlu N. Chest trauma: analysis of 592 cases. Ulus Travma Acil Cerrahi Derg 2003; 9: 275-80.
4) Başoğlu A, Akdağ AO, Çelik B, Demircan S. Thoracic trauma: an analysis of 521 patients. Ulus Travma Acil Cerrahi Derg 2004; 10: 42-6.
5) LoCicero J 3rd, Mattox KL. Epidemiology of chest trauma. Surg Clin North Am 1989; 69: 15-9.
6) Sırmalı M, Türüt H, Topçu S, Gülhan E, Yazıcı U, Kaya S, et al. A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardiothorac Surg 2003; 24: 133-8.
7) Robison PD, Harman PK, Trinkle JK, Grover FL. Management of penetrating lung injuries in civilian practice. J Thorac Cardiovasc Surg 1988; 95: 184-90.
8) Molnar TF. Surgical management of chest wall trauma. Thorac Surg Clin 2010; 20: 475-85.



