

2Department of Thoracic Surgery, Mardin State Hospital, Mardin, Turkey
3Department of Thoracic Surgery Burdur State Hospital, Burdur, Turkey
4Department of Thoracic Surgery, İstinye University, Liv Hospital, Istanbul, Turkey DOI : 10.26663/cts.2019.00028
Summary
Intrathoracic splenosis presents a rare thoracic lesion occurring after splenectomy or abdominal trauma as a consequence of heterotopic autotransplantation and implantation of splenic tissue. We present a 38- yearold man with intrathoracic splenosis. He was admitted to hospital with chest pain. In computed tomography homogenous, smooth-edged multiple lesions were found. The patient was not able to be diagnosed with transthoracic fine needle aspiration biopsy. On the exploration, there were multiple lesions at the thoracic cavity and the masses were excised. Definitive pathology was reported as splenosis.Introduction
Thoracic splenosis (TS) is a rare condition following diaphragmatic injury or an abdominal surgery, with autotransplantation of splenic tissue into the left hemithorax. TS typically presents in the chest radiography as solitary or multiple lung masses and the diagnosis is challenging if history of a previous abdominal injury is not obtained. Herein, we present a rare case of thoracic splenosis diagnosed 4 years after an abdominal trauma.Case Presentation
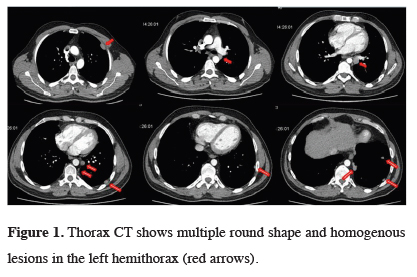
A 38-year-old male patient admitted to the hospital with chest pain. On the posterior-anterior chest X-ray, there were homogeneous opacities in the middle zone and diaphragmatic pleura of the left hemithorax. On the computerized thorax tomography (CT), homogeneous, smooth-edged multiple lesions were found in the lower lobe of the left lung, including parenchymal, costal, and diaphragmatic pleura (largest diameter of 3.5 cm) (Figure 1). In positron emission tomography, FDG uptake level of the lesion was 2.5.
 Click Here to Zoom |
Figure 1: Thorax CT shows multiple round shape and homogenous lesions in the left hemithorax (red arrows). |
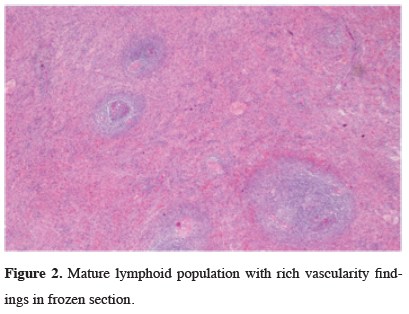
Transthoracic fine needle aspiration biopsy was not diagnostic. We decided to perform an exploratory video-assisted thoracoscopic surgery (VATS) for the diagnosis and treatment. However, it was converted to a thoracotomy due to excessive adhesions. Upon exploration, multiple lesions on the chest wall, aortic adventitia, and lung parenchyma were observed. Excisional biopsy of one of the lesions performed and the frozen section reported a collection of lymphoid cells in the vasculature pattern and benign/malign discrimination could not be done on histopathological examination. All masses was resected from the defined regions report.
The final pathology examination of the specimens revealed that, there was perivascular mature lymphocyte population that formed nodules in the roof with rich interstitial vascularity which was compatible with typical spleen morphology (Figure 2). When the patient’s anamnesis was detailed, a history of blunt trauma to the abdominal region, which was medically treated 4 years ago, was found.
 Click Here to Zoom |
Figure 2: Mature lymphoid population with rich vascularity findings in frozen section. |
Discussion
Accessory spleens and splenosis are two distinct forms of ectopic splenic tissue which might be found in the body. During the embryological period of development accessory spleens arise from the left side of the dorsal mesogastrium and moves to abnormal localizations. On the other hand splenosis is autotransplantation of splenic tissue through different anatomical localizations of the human body and it generally occurs after trauma, surgery or iatrogenic rupture of the spleen[1].Shaw et al [2] reported for the first time in 1937 that splenic tissue autotransplantation after splenectomy to the thoracic cavity resulted in an incidence of TS. In 2016, Tulinský et al [3] stated that there were 75 patients in the English literature. A total of 81 cases were published until now. Most of the patients had abdominal trauma in their history. The splenic nodules may be few or up to hundreds in the peritoneal cavity and can be localized in the splenic bed, omentum, mesentery, liver, or diaphragm [4]. Splenic tissue could be found in intraperitoneal or extraperitoneal locations. Splenosis has also been reported rarely in the pericardium, subcutaneous tissue and even in the occipital pole of the brain [1].
The time interval between abdominal injury requiring splenectomy and thoracic splenosis detection varies from several years to decades [3]. Most patients with splenosis are asymptomatic, but 10-15% of them may have pleuritic pain, pleurisy, recurrent hemothorax, or fever [3]. Patients with a diaphragm, phrenic nerve, and parietal pleural involvement may have pain. Our patient was symptomatic because of the location of lesions.
The differential diagnosis of intrathoracic splenosis includes lung carcinomas, pleural metastases, lymphoma, malignant mesothelioma, invasive thymoma, gossypiboma and fibrous tumors of the pleura. Scintigraphy with Tc-99m-labeled and heat-altered erythrocyte is the gold standard method [5,6]. Thorax CT shows a well-defined, homogeneous, pleural-based nodule in the left hemithorax [7,8]. Thorax CT of our patient had multinodular, well-defined masses in the lung. It is not necessary to surgically treat patients who are suspected of TS in the preoperative period.
A 99 m technetium‐labeled heat‐damaged red cell scan is highly specific for detection of splenosis and considered as the gold standard, due to reduced uptake in the normal liver. With the emergence of improved resolution of planar/single photon emission computed tomography/computed tomography (SPECT/CT) scans, Tc‐99 m sulphur colloid scintigraphy can be a reliable for differentiating splenic tissue from non‐splenic tissue [7,9].
Especially in splenectomy patients, surgical resection is unnecessary. Surgical resection should be considered only in symptomatic patients. In our 6 months follow-up after discharge, the patient’s pain was ceased. If there are difficulties in diagnosing on left lower zone lesions, the history of trauma and splenectomy should be questioned in carefully.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Reference
1) Fremont RD, Rice TW. Splenosis: a review. South Med J 2007; 100: 589-94.
2) Bernard Shaw AF, Shafi A. Traumatic autoplastic transplantation of splenic tissue in man with observations on the late results of splenectomy in six cases. J Pathol 1937; 45: 215-35.
3) Tulinský L, Ihnát P, Mitták M, Guňková P, Zonča P. Intrathoracic splenosis–lesson learned: a case report. J Cardiothorac Surg 2016; 11: 72.
4) Kumbasar U, Döner E, Enön S, Akal M, Öztürk C. Thoracic splenosis. Turk J Haematol 2005; 22: 147-9.
5) Armas RR. Clinical studies with spleen-specific radiolabeled agents. Semin Nucl Med 1985; 15: 260-75.
6) Cansever L, Ceyhan S, Kutluk AC, Seyrek Y, Atabey F, Fener NA et al. Thoracic splenosis after thoracoabdominal injury sustained 25 years previously. Curr Thorac Surg 2017; 2: 70-2.
7) Aggarwal R, Wagner T, Navalkissoor S. Case Report of Tc-99m Sulfur Colloid Single-Photon Emission Computed Tomography/Computed Tomography Study Differentiating Tumor from Accessory Spleen. World J Nucl Med 2013; 12: 129.



