2Department of Thoracic Surgery, Medicana Hospital, Izmir, Turkey DOI : 10.26663/cts.2023.0026
Summary
Immunotherapy is gaining increasing attention as a neoadjuvant therapy for resectable non-small cell lung cancer (NSCLC). We report a case with second primary lung adenocarcinoma that was applied via video-assisted thoracoscopic surgery (VATS) lobectomy with guillotine stapler technique after treatment with immunotherapy in combination with chemotherapy. Although surgery is challenging after immunotherapy, this particular case showed that the VATS approach may be safe and feasible in experienced hands.Introduction
Immunotherapy has achieved great success in treating lung cancer. Three major immunotherapy treatment modalities mentioned in the literature are immunomodulatory antibodies, chimeric antigen receptors (CARs) and vaccines [1]. Immune checkpoint inhibitors (ICIs) for advanced lung cancer are gaining increasing attention as a neoadjuvant therapy for resectable non-small cell lung cancer (NSCLC). Meanwhile, data regarding the safety and feasibility of surgical resection after treatment with immunotherapy for NSCLC remains scarce.We report a case with second primary lung adenocarcinoma who was operated via video-assisted thoracoscopic surgery (VATS) lobectomy with guillotine stapler technique after treatment with immunotherapy in combination with chemotherapy.
Case Presentation
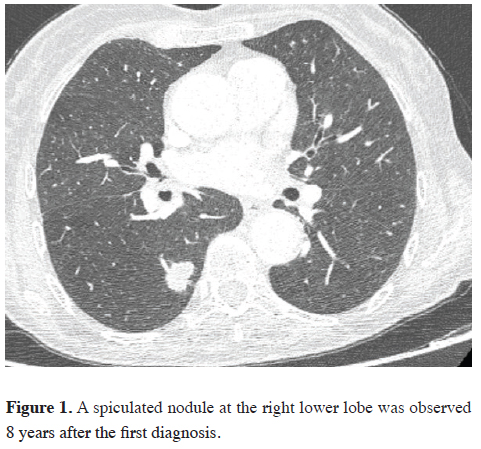
A 61-year-old female patient admitted to our hospital in 2014 with complaints of hip pain, cough and shortness of breath. Computed tomography images revealed lytic bone metastasis in the left acetabulum and a mass invading the mediastinum in the upper lobe of the right lung. On PET imaging, a mass of 3.5 cm in size, showing 15.6 FDG uptake, invading the mediastinum narrowing the right upper lobe bronchus, multiple mediastinal hypermetabolic lymphadenopathy and left iliac bone metastasis were observed. The patient was diagnosed as stage IV lung adenocarcinoma after a bronchoscopic biopsy. She had severe pain following radiotherapy and zoledronic acid treatment for acetabular bone metastasis, and she was operated on for hip arthroplasty. Postoperative bone pathology was reported as metastatic adenocarcinoma of the lung. After 3 cycles of carboplatin and pemetrexed chemotherapy, three cycles of docetaxel chemotherapy was given due to the progression of the lung mass. Nivolumab immunotherapy, a PD-1 blocking agent, which is one of the checkpoint inhibitors, was started for the patient whose tumor size continued to increase. In the imaging after 10 cycles of treatment, the tumor in the upper lobe of the right lung was observed to regress almost completely. In the CT scan of the patient in the year 2022, after eight years from the first diagnosis with the complaint of cough and three years since the last nivolumab dose usage, a 20x13 mm spiculated nodule at the right lung lower lobe was observed (Figure 1). The SUVmax value of the nodule was 9.2 on PET-CT and no metastasis was detected on the remaining body parts. The Patient was prepared for VATS lobectomy. Pathological result by frozen section confirmed NSCLC. On exploration, there were very dense pleural adhesions and severe tissue fibrosis on the hilum thought to be due to immuno-chemotherapy causing a very difficult and dangerous dissection. After division of the inferior pulmonary vein, the lower lobe artery and lower lobe bronchus, which were “fusioned” were dissected and divided together with an endostapler using the “guillotine stapler technique’’[2]. The middle lobe bronchus was protected by transillumination of the fiber optic bronchoscope delivered through the endobronchial tube from the surgical field. Lymph node dissection was difficult due to mediastinal rigidity. After the surgical procedure, the patient had an uneventful recovery and was discharged from the hospital on the fifth postoperative day. The pathological diagnosis was secondary primary lung adenocarcinoma (T1cN0M0, Stage IA3). Written informed consent was obtained from the patient for the publication of her data.
 Click Here to Zoom |
Figure 1: A spiculated nodule at the right lower lobe was observed 8 years after the first diagnosis. |
Discussion
There are several advantages of neoadjuvant therapy, e.g., increasing the resectability by downstaging the lung tumors, improving the rate of lung sparing surgery, and increasing distant and local disease control [3]. Immune checkpoint inhibitors (ICIs) such as atezolizumab, durvalumab, nivolumab, and pembrolizumab have been approved for first- or second-line use in patients with metastatic NSCLC or selected stage III locally advanced NSCLC. Neoadjuvant ICIs are currently being evaluated alone or in combination with chemotherapy in many clinical trials in patients with diverse tumor types [4]. However, the risks of disease progression before surgery, delays to resection, perioperative morbidity and mortality, and their impact on intraoperative technical difficulty after neoadjuvant ICIs are still poorly understood. Although the therapeutic value of resecting residual primary or metastatic foci remains controversial in general, the safety and feasibility of pulmonary resection after treatment with immunotherapy agents, in particular, have not yet been studied. Benign lung diseases, secondary infections, malignancy itself, chemotherapy, radiation and immunotherapy as a neoadjuvant therapy can usually be accompanied by inflammation as a result, peribronchial conglomerated lymph nodes, adhesions and fusion between the artery and bronchus, and hypertrophy of the bronchial arteries may occur [2]. In these cases, there is a high risk of complications, such as bleeding during hilum dissection. In our case, very dense adhesion between the artery and bronchus and the rigid connective tissue were the challenging parts of the surgery which led us to choose the guillotine technique. Minimally invasive approaches are feasible in this patient population, but may be more difficult than in cases without neoadjuvant immunotherapy. Operations may be challenging, owing to post-treatment adhesions and the surgeon has to be aware and converting to open thoracotomy may be necessary. Resection after neoadjuvant ICI may increase intraoperative technical difficulty because of inflammation-induced perihilar or lobar dense fibrosis and lymphadenopathy. Due to these difficulties conversion rates of up to 54% have been reported in the literature. The optimal timing of surgery after neoadjuvant immunotherapy is undetermined but most studies scheduled resection approximately 3 to 6 weeks after treatment [5].In conclusion we reported a case of right lower lobectomy due to second primary lung adenocarcinoma in a patient who received long term immunotherapy after her first primary. Although surgery is challenging after immunotherapy, this particular case showed that the VATS approach may be safe and feasible in experienced hands. The use of the guillotine technique may be necessary for patients having strong adhesions between pulmonary artery and bronchus to avoid injury to vascular structures and bleeding. By cutting the artery-bronchus complex, transillumination of the fiberoptic bronchoscope should be used to check that the middle lobe bronchus on the right side and the upper lobe bronchus on the left side are not obliterated. There is insufficient information about the long-term fistula risk of the guillotine technique in the literature. Therefore, this technique should be applied carefully with the results in mind.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect
to the authorship and/or publication of this article.
Funding
The authors received no financial support.
Authors’ contributions
DG,ÖS,KT: conceived and designed the current case
report, co-wrote the paper, collected the clinical data.
The authors discussed the case under the literature data
together and constituted the final manuscript.
Reference
1) Lohmueller J, Finn OJ. Current modalities in cancer immunotherapy:
Immunomodulatory antibodies, CARs and vaccines.
Pharmacol Ther 2017; 178: 31-47.
2) Yıldıran H, Sunam GS. A different approach in thoracic surgery:
Guillotine lobectomy. Turk Gogus Kalp Dama 2021; 29: 520-6.
3) Xu K, Yang H, Ma W, Fan L, Sun B, Wang Z, Al-Hurani MF
et al. Neoadjuvant immunotherapy facilitates resection of surgically-
challenging lung squamous cell cancer. J Thorac Dis
202; 13: 6816-26.






